Diabetes Reversal
UNIT 1 |
OBJECTIVES
REFERENCE
- To Identify types of Diabetes
- To discuss potential complications of diabetes
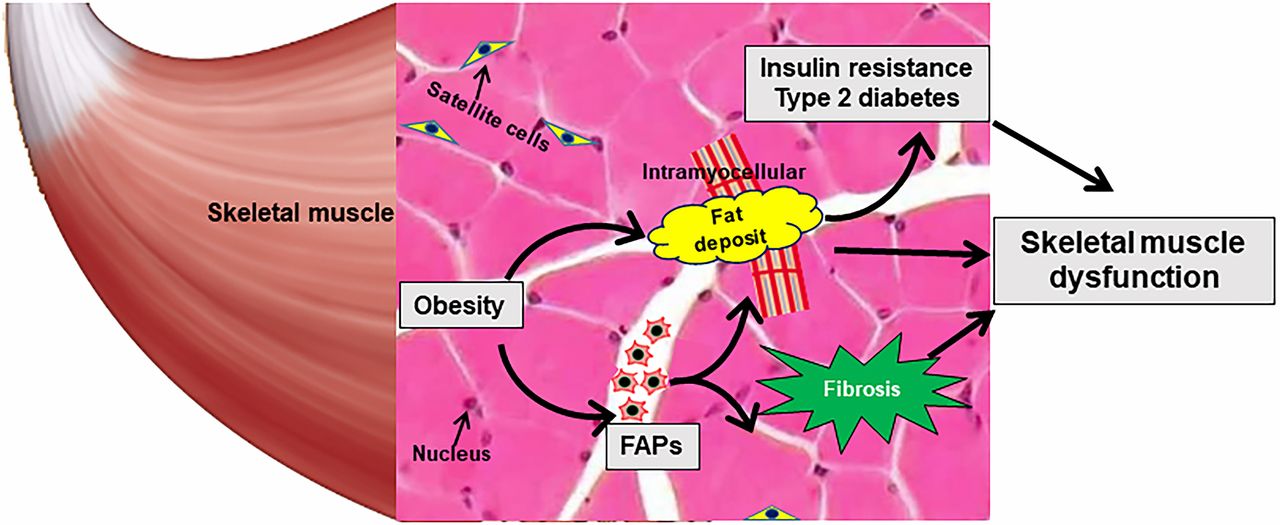
- Learn how Lipotoxicity in Skeletal muscle affects insulin resistance
- Discuss the Dysbiosis, Glucotoxicity and Diabetes
REFERENCE
- Kick Diabetes Essentials, Brenda Davis, RD
- Nutrition Facts, Michael Greger, MD
What is Diabetes?
Diabetes is a group of diseases characterized by high blood glucose (sugar) levels. If you have diabetes, your body fails to produce enough insulin and may also fail to properly use the insulin it produces. Insulin is the hormone you need so your cells can convert glucose (a sugar that's the body's main source of fuel) into energy. Insulin does this by attaching to receptor sites on your cells (like a key in a lock) and sending signals to open the gates so glucose can enter the cells. When insulin isn't present or doesn't do its job, sugar accumulates in the blood, resulting in high blood sugar (hyperglycemia). Some sugar also spills out into your urine. When diabetes was first discovered, it was diagnosed by tasting a patient's urine. If it tasted sweet, this was a sign that death was imminent. Fortunately, the prognosis changed dramatically with the discovery of insulin in 1921. There are three main types of diabetes: type l, type 2, and gestational diabetes.
Type 1 Diabetes
Type 1 diabetes is an autoimmune disease. The body mistakes the cells in the pancreas that manufacture insulin (beta cells) for foreign invaders and generates chemicals to destroy them. The insulin-making machine is disabled, so little or no insulin is produced. In some cases, a persons genetics could be responsible for this condition. In others, viral infections or environmental contaminants may trigger this abnormal immune response. A third possibility is that certain food proteins that find their way into the bloodstream are the culprits. These proteins are so similar to pancreatic beta cell proteins that the body attacks both. Specific types of dairy protein lit this bill, and introduction to whole cow's milk at a very early age appears particularly problematic, especially in infants and children who are genetically susceptible.
Type l diabetes was formerly referred to as juvenile-onset diabetes or insulin-dependent diabetes mellitus because it occurs mostly in children or young adults. However, adults over the age of thirty occasionally develop type I diabetes. This type of diabetes is called latent autoimmune diabetes in adults (LADA) and is sometimes also referred to as type l.5 diabetes. Adults diagnosed with LADA are often not overweight and have little or no resistance to insulin (the body is able to use insulin when it is present). They also often have a slower rate of beta cell failure and thus may not need insulin as quickly as younger individuals with more aggressive disease. LADA is more common than previously recognized, accounting for an estimated 2-12 percent of diabetes in the adult population. Individuals with LADA can be distinguished from those with type 2 diabetes by the presence of autoantibodies (antibodies that are directed against one or more of the body's own proteins) associated with type 1 diabetes. People with type 1 diabetes rely on daily insulin injections for survival. It's possible for people with type 1 diabetes to develop type 2 diabetes if their body becomes insulin resistant. Only 5-10 percent of people with diabetes suffer from type 1.
Type 2 Diabetes
Type 2 diabetes is a disease of insulin resistance and reduced production of insulin by the pancreas. While either of these metabolic abnormalities can result in full-blown type 2 diabetes, in the majority of affected individuals, both are present. Insulin resistance is a condition in which the body's cells are insensitive or resistant to the insulin it produces. In other words, insulin is made, but it can't do its job moving glucose into cells or it does the job inefficiently. The natural consequence of insulin resistance is elevated blood glucose. The pancreas responds by putting out more insulin, which shifts the beta cells into overdrive. Insulin resistance is generally present for many years prior to the diagnosis and is a key feature of prediabetes.
Type 1 Diabetes
Type 1 diabetes is an autoimmune disease. The body mistakes the cells in the pancreas that manufacture insulin (beta cells) for foreign invaders and generates chemicals to destroy them. The insulin-making machine is disabled, so little or no insulin is produced. In some cases, a persons genetics could be responsible for this condition. In others, viral infections or environmental contaminants may trigger this abnormal immune response. A third possibility is that certain food proteins that find their way into the bloodstream are the culprits. These proteins are so similar to pancreatic beta cell proteins that the body attacks both. Specific types of dairy protein lit this bill, and introduction to whole cow's milk at a very early age appears particularly problematic, especially in infants and children who are genetically susceptible.
Type l diabetes was formerly referred to as juvenile-onset diabetes or insulin-dependent diabetes mellitus because it occurs mostly in children or young adults. However, adults over the age of thirty occasionally develop type I diabetes. This type of diabetes is called latent autoimmune diabetes in adults (LADA) and is sometimes also referred to as type l.5 diabetes. Adults diagnosed with LADA are often not overweight and have little or no resistance to insulin (the body is able to use insulin when it is present). They also often have a slower rate of beta cell failure and thus may not need insulin as quickly as younger individuals with more aggressive disease. LADA is more common than previously recognized, accounting for an estimated 2-12 percent of diabetes in the adult population. Individuals with LADA can be distinguished from those with type 2 diabetes by the presence of autoantibodies (antibodies that are directed against one or more of the body's own proteins) associated with type 1 diabetes. People with type 1 diabetes rely on daily insulin injections for survival. It's possible for people with type 1 diabetes to develop type 2 diabetes if their body becomes insulin resistant. Only 5-10 percent of people with diabetes suffer from type 1.
Type 2 Diabetes
Type 2 diabetes is a disease of insulin resistance and reduced production of insulin by the pancreas. While either of these metabolic abnormalities can result in full-blown type 2 diabetes, in the majority of affected individuals, both are present. Insulin resistance is a condition in which the body's cells are insensitive or resistant to the insulin it produces. In other words, insulin is made, but it can't do its job moving glucose into cells or it does the job inefficiently. The natural consequence of insulin resistance is elevated blood glucose. The pancreas responds by putting out more insulin, which shifts the beta cells into overdrive. Insulin resistance is generally present for many years prior to the diagnosis and is a key feature of prediabetes.
What commonly triggers the progression to type 2 diabetes is that, in addition to insulin resistance, the insulin-producing beta cells begin to fail and the amount of insulin produced declines. This failure may well be the result of beta cell exhaustion. By the time a person is diagnosed, insulin production has commonly diminished to about 50 percent of normal, although in some individuals insulin production remains high. Although insulin resistance tends to remain relatively constant over time, a steady decline in insulin production generally continues if changes in diet and lifestyle are not made. Type 2 diabetes was once known as adult-onset diabetes or non-insulin-dependent diabetes mellitus, as it was a disease that occurred almost exclusively in adults. Although exceedingly rare prior to the twentieth century, today type 2 diabetes is a global epidemic and accounts for 90-95 percent of all diabetes. While type 2 diabetes was once unheard of in young people, it now accounts for 20-50 percent of diabetes in youth.
Gestational Diabetes
Gestational diabetes is a temporary condition during pregnancy that is often resolved with the birth of the infant. Its incidence has risen from 3-5 percent of pregnancies or to the twenty-first century to 5-10 percent today. An estimated 50 percent of women with gestational diabetes go on to develop type 2 diabetes.
How Type 2 Diabetes Diagnosed?
Type 2 diabetes may be suspected it you experience the following common
symptoms of the disease:
Gestational Diabetes
Gestational diabetes is a temporary condition during pregnancy that is often resolved with the birth of the infant. Its incidence has risen from 3-5 percent of pregnancies or to the twenty-first century to 5-10 percent today. An estimated 50 percent of women with gestational diabetes go on to develop type 2 diabetes.
How Type 2 Diabetes Diagnosed?
Type 2 diabetes may be suspected it you experience the following common
symptoms of the disease:
- Blurred vision
- Fatigue
- Itchy skin
- Pain, numbness, or pain in extremities
- Polydipsia (constant thirst)
- Polyphagia (increased hunger)
- Polyuria (frequent urination)
- Recurrent infections
- Slow wound healing
- Sudden, unexpected weight loss
1. Fasting plasma glucose. After at least eight hours (nothing by mouth except water), your blood sugar is tested, your fasting blood glucose results will determine whether or not you have diabetes or prediabetes.
DIAGNOSIS |
FASTING PLASMA GLUCOSE |
Diabetes |
126 mg/dL (7.0 mmol/L) or higher |
Prediabetes |
100-125 mg/dL (5.6 to 6.9 mmol/L) |
Normal |
60-99 mg/dL (3.3 to 5.5 mmol/L) |
2. Alc (or HbAlc). This is a blood test that provides information about your average blood sugar levels over the past two to three months, It measures the percentage of blood sugar attached to hemoglobin (the oxygen-carrying protein in red blood cells). The result is reported as a percentage.
Diagnosis |
A1c |
Diabetes |
6.5% or more |
Prediabetes |
5.7-6.4% |
Normal |
Less than 5.7% |
3. Oral glucose tolerance test. This test measures how well your body uses sugar. You fast overnight and then drink a sugary liquid (glucose dissolved in water). Your blood sugar is then measured periodically over the next two hours.
Diagnosis |
Oral Glucose Tolerance Test At Two Hours |
200 mg/dL (11.1 mmol/L) or higher |
|
140-199 mg/dL (7.8-11.0 mmol/L) |
|
140 mg/dL (7.8 mmol/L) or less |
4. Random plasma glucose. This is a random measure of your sugar level at any time during the day, irrespective of the time of your last meal. A random plasma glucose level of 200 mg/dL. (11.1 mmo/L) or higher suggests diabetes.
Complications of Diabetes
Insulin resistance, rising blood sugar, and diabetes come with a dreadful physiological price tag. Living in a milieu of excess glucose, your tissues become awash in a syrupy fluid. The sugars stick to proteins, bridging spaces between connective tissue layers. Arteries stiffen, the lenses of the eyes become less flexible, internal wiring malfunctions, and aging accelerates. Every body system is affected, and the consequence is a metabolic meltdown. As a result, people with diabetes have a two to threefold increase in risk of mortality compared with those who do not have diabetes. The devastation wrought by diabetes is responsible for a myriad of complications.
Cardiovascular Disease
According to the American Heart Association, about 84 percent of people age sixty-five or older with diabetes die from heart disease or stroke. Adults with diabetes are two to four times more likely to die from heart disease or heart failure than adults without diabetes. This is thought to be because people with diabetes have more hypertension; higher levels of cholesterol, triglycerides, and blood glucose; increased rates of obesity; and tend to be less physically active. Deaths from cardiovascular disease also occur at earlier ages than they do in people who do not have diabetes.
According to the American Heart Association, about 84 percent of people age sixty-five or older with diabetes die from heart disease or stroke. Adults with diabetes are two to four times more likely to die from heart disease or heart failure than adults without diabetes. This is thought to be because people with diabetes have more hypertension; higher levels of cholesterol, triglycerides, and blood glucose; increased rates of obesity; and tend to be less physically active. Deaths from cardiovascular disease also occur at earlier ages than they do in people who do not have diabetes.
Peripheral Artery Disease (PAD)
An estimated 10-20 percent of people with diabetes suffer from peripheral artery disease (PAD), with its incidence increasing with age. This condition is marked by narrowing of the arteries to the legs, stomach, arms, and head caused by atherosclerosis. Diabetic foot ulcers resulting from PAD are also a common complication, with 12-25 percent of people with diabetes being allected in their lifetime.
An estimated 10-20 percent of people with diabetes suffer from peripheral artery disease (PAD), with its incidence increasing with age. This condition is marked by narrowing of the arteries to the legs, stomach, arms, and head caused by atherosclerosis. Diabetic foot ulcers resulting from PAD are also a common complication, with 12-25 percent of people with diabetes being allected in their lifetime.
Peripheral Neuropathy
Diabetes can damage nerves and cause pain in the limbs, especially in the legs, feet, and hands. This impairs feeling and makes it easy to miss small injuries that can become infected. If left unchecked, peripheral neuropathy can lead to serious infections. Diabetes is responsible for about 60 percent of nontraumatic, lower-limb amputations among adults age twenty or older.
Diabetes can damage nerves and cause pain in the limbs, especially in the legs, feet, and hands. This impairs feeling and makes it easy to miss small injuries that can become infected. If left unchecked, peripheral neuropathy can lead to serious infections. Diabetes is responsible for about 60 percent of nontraumatic, lower-limb amputations among adults age twenty or older.
Kidney Disease
In 2011 and 2012, the prevalence of chronic kidney disease in American adults with diabetes was 36.9 percent, and diabetes was the main cause of kidney failure in 44 percent of new cases.
Cancer
Diabetes is positively associated with overall cancer risk, particularly cancers of the pancreas (1.94 times the risk), colon (1.38 times the risk), rectum (1.2 times the risk), liver (2.2 times the risk), and endometrium (2.1 times the risk). In a 2018 American study, people with diabetes had a 47 percent greater chance of having colorectal cancer (CRC) than individuals without the disease. Although the increase in CRC risk was no significant in people age sixty-five or older, the odds of developing the disease in those younger than sixty-five were nearly five times greater than those without diabetes.
In 2011 and 2012, the prevalence of chronic kidney disease in American adults with diabetes was 36.9 percent, and diabetes was the main cause of kidney failure in 44 percent of new cases.
Cancer
Diabetes is positively associated with overall cancer risk, particularly cancers of the pancreas (1.94 times the risk), colon (1.38 times the risk), rectum (1.2 times the risk), liver (2.2 times the risk), and endometrium (2.1 times the risk). In a 2018 American study, people with diabetes had a 47 percent greater chance of having colorectal cancer (CRC) than individuals without the disease. Although the increase in CRC risk was no significant in people age sixty-five or older, the odds of developing the disease in those younger than sixty-five were nearly five times greater than those without diabetes.
Cognitive Dysfunction
Vascular dementia and Alzheimer's disease are frequently seen in diabetes sufferers. One recent meta-analysis (combined findings) of seventeen studies involving close to two million individuals reported that participants with diabetes had a 1.54 times increased risk of Alzheimer's disease."
Vascular dementia and Alzheimer's disease are frequently seen in diabetes sufferers. One recent meta-analysis (combined findings) of seventeen studies involving close to two million individuals reported that participants with diabetes had a 1.54 times increased risk of Alzheimer's disease."
Other Conditions
Diabetic retinopathy, a complication of diabetes that involves damage to the retinal blood vessels, is the leading cause of blindness in American adults. It's estimated to impact over 25 percent of Americans with type 2 diabetes. Also, a 2018 study of Chinese men reported that almost 65 percent of patients with diabetes suffered from erectile dysfunction (ED). Finally, diabetes is strongly associated with the risk and severity of depression. Depression is present in about 25 percent of people with type 2 diabetes.
All in all, these complications pose a rather gloomy reality tor anyone progressing down the very slippery slope of diabetes. Fortunately, all these conditions can be dramatically diminished, halted in their tracks, or even reversed with appropriate diet and lifestyle changes.
Diabetic retinopathy, a complication of diabetes that involves damage to the retinal blood vessels, is the leading cause of blindness in American adults. It's estimated to impact over 25 percent of Americans with type 2 diabetes. Also, a 2018 study of Chinese men reported that almost 65 percent of patients with diabetes suffered from erectile dysfunction (ED). Finally, diabetes is strongly associated with the risk and severity of depression. Depression is present in about 25 percent of people with type 2 diabetes.
All in all, these complications pose a rather gloomy reality tor anyone progressing down the very slippery slope of diabetes. Fortunately, all these conditions can be dramatically diminished, halted in their tracks, or even reversed with appropriate diet and lifestyle changes.
The Making of Diabetes
The hallmark of our modern type 2 diabetes epidemic is INSULIN RESISTANCE. Even when adequate insulin is produced by the beta cells of the pancreas, the body cells (regardless of whether they're in muscle, liver, or fat tissue) do not respond to the insulin as they should. This can happen when there's a problem with insulin receptors or a glitch in the mechanisms that work together to move glucose into ceils. Even with plenty of insulin in the bloodstream, glucose can't get into the cells to be used for energy. This means that sugar accumulates in the bloodstream, causing high blood sugar hyperglycemia). The pancreas responds to this surge in blood sugar by supplying even more insulin. This chronic excess of insulin circulating in the bloodstream is known as hyperinsulinemia. To be clear, insulin is an extremely important hormone in the body, helping to regulate many body systems. However, like all hormones, there's an optimal level of insulin that's needed to maintain health. When insulin in the bloodstream is persistently elevated and the body is resistant to that insulin, a metabolic mess ensues. Chronically high insulin levels can lead to weight gain, high triglyceride and uric acid levels, arteriosclerosis (hardening of the arteries), hypertension, and endothelial dysfunction (which impairs blood flow).
What Causes Insulin Resistance?
The vast majority of insulin resistance is a function of overweight and underactivity. While it's true that genes can be responsible for ineffective insulin receptor sites or can adversely affect the cascade of events necessary for glucose to enter cells, excess body weight, especially visceral fat, is the chief culprit.
According to the International Diabetes Federation, a waist measurement of 37 inches (94 cm) or more in Caucasian men, 35.5 inches or more in Asian men, and 31.5 inches or more in women increases risk. Underactivity contributes to being overweight and to metabolic changes that further promote insulin resistance.
With unhealthy eating patterns, chronic overeating, and underactivity (and the overweight or obesity that results), metabolic mayhem ensues. This, in turn, incites five major drivers of insulin resistance and diabetes: inflammation, oxidative stress, lipotoxicity, glycotoxicity, and dysbiosis.
The vast majority of insulin resistance is a function of overweight and underactivity. While it's true that genes can be responsible for ineffective insulin receptor sites or can adversely affect the cascade of events necessary for glucose to enter cells, excess body weight, especially visceral fat, is the chief culprit.
According to the International Diabetes Federation, a waist measurement of 37 inches (94 cm) or more in Caucasian men, 35.5 inches or more in Asian men, and 31.5 inches or more in women increases risk. Underactivity contributes to being overweight and to metabolic changes that further promote insulin resistance.
With unhealthy eating patterns, chronic overeating, and underactivity (and the overweight or obesity that results), metabolic mayhem ensues. This, in turn, incites five major drivers of insulin resistance and diabetes: inflammation, oxidative stress, lipotoxicity, glycotoxicity, and dysbiosis.
Inflammation
We're all familiar with the heat, redness, swelling, and pain associated with an injury or a sore throat; this is the result of inflammation. Inflammation is the body's way of getting rid of damaged cells and initiating tissue repair. However, there's a type of inflammation associated with many chronic diseases (including type 2 diabetes) that can't be seen or felt. It can be fueled by an unhealthy diet, food sensitivities, dysbiosis, alcohol, and overweight. Excess body fat, especially visceral fat, causes the release of cell-signaling proteins called cytokines that can trigger inflammation. This inflammation reduces insulin's ability to send messages to the cell to open the glucose gates. Body cells become less responsive to insulin, ultimately increasing insulin resistance. Insulin resistance itself causes inflammation, so a positive feedback loop is reinforced.
Oxidative Stress
Oxidative stress, or oxidation, is an imbalance between substances called pro-oxidants (such as free radicals) and antioxidants. Free radicals are unstable molecules that have an electron that is unpaired. They try to stabilize by stealing electrons from other molecules. When they succeed, they turn their victim into a tree radical, setting off a destructive chain reaction that creates more free radicals. Antioxidants are heroes that block the chain of destruction by offering the free radical an electron without becoming free radicals themselves.
Increased oxidative stress has been shown to promote insulin resistance and malfunction of the pancreatic cells that produce insulin. When you eat too much and exercise too little, you end up with an over load of sugar and fat. Excess sugar can bind to proteins, forming advanced glycation end products (AGEs), which accelerate the production of free radicals. AGEs alter cell function, disrupt insulin receptors, in crease insulin resistance, and promote inflammation.
We're all familiar with the heat, redness, swelling, and pain associated with an injury or a sore throat; this is the result of inflammation. Inflammation is the body's way of getting rid of damaged cells and initiating tissue repair. However, there's a type of inflammation associated with many chronic diseases (including type 2 diabetes) that can't be seen or felt. It can be fueled by an unhealthy diet, food sensitivities, dysbiosis, alcohol, and overweight. Excess body fat, especially visceral fat, causes the release of cell-signaling proteins called cytokines that can trigger inflammation. This inflammation reduces insulin's ability to send messages to the cell to open the glucose gates. Body cells become less responsive to insulin, ultimately increasing insulin resistance. Insulin resistance itself causes inflammation, so a positive feedback loop is reinforced.
Oxidative Stress
Oxidative stress, or oxidation, is an imbalance between substances called pro-oxidants (such as free radicals) and antioxidants. Free radicals are unstable molecules that have an electron that is unpaired. They try to stabilize by stealing electrons from other molecules. When they succeed, they turn their victim into a tree radical, setting off a destructive chain reaction that creates more free radicals. Antioxidants are heroes that block the chain of destruction by offering the free radical an electron without becoming free radicals themselves.
Increased oxidative stress has been shown to promote insulin resistance and malfunction of the pancreatic cells that produce insulin. When you eat too much and exercise too little, you end up with an over load of sugar and fat. Excess sugar can bind to proteins, forming advanced glycation end products (AGEs), which accelerate the production of free radicals. AGEs alter cell function, disrupt insulin receptors, in crease insulin resistance, and promote inflammation.
|
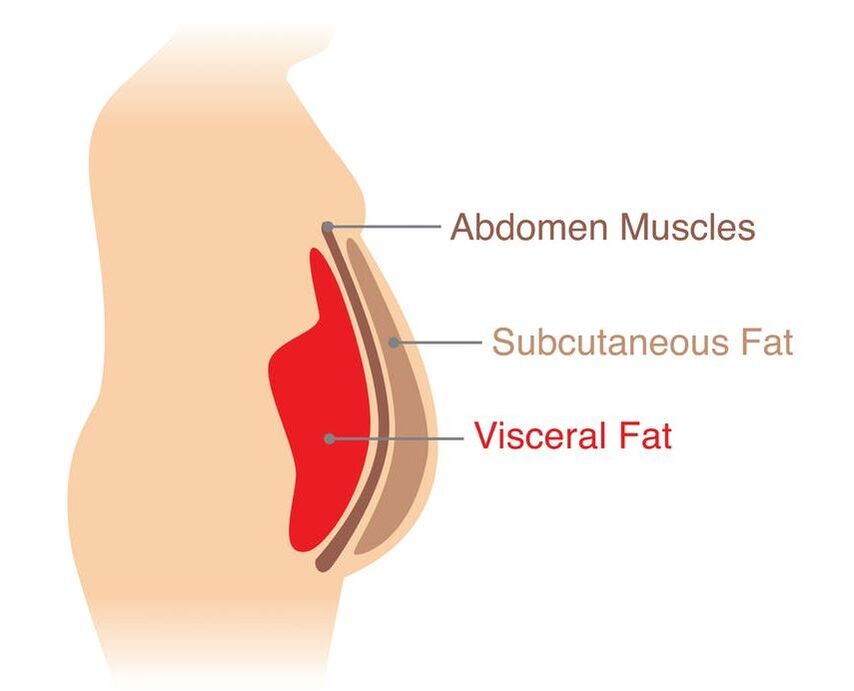
VISCERAL FAT
When fat is stored just below the surface of the skin, it's called subcutaneous fat. When it's found deep within the body, in and around vital organs, its called visceral fat. Generally, people with an apple shape (more fat in their abdomen) have more visceral fat, and those who are pear shaped (more fat in the extremities, such as hips and thighs) have more subcutaneous fat. However, even among individuals who are apple shaped, there are significant differences in the distribution of visceral versus subcutaneous fat. |
People with soft bellies tend to have more subcutaneous fat, while those with big, hard bellies have more visceral fat. While all types of excess fat can adversely affect health, visceral fat is by far the most concerning. This is because it's much more biologically active than subcutaneous fat, pumping out an inflammatory set of hormones called cytokines and free fatty acids that disrupt normal metabolism. This, in turn, increases insulin resistance and the risk of heart disease, hypertension, and some types of cancers.
However, when calorie intake chronically exceeds expenditure, the storage process can back up; excess fatty acids will be stored directly in the liver or be shuttled to the pancreas, heart, or muscle tissue. Over accumulation of fatty acids disrupts the normal workings of these cells, often leading to cell damage or cell death. Vital organs are especially vulnerable because they're highly specialized systems that can't tolerate a significant infiltration of fatty acids. When fat is stored in the liver, it becomes less sensitive to insulin, promoting insulin resistance throughout the body. The pancreas has a particularly low tolerance for fat, so even a small exposure can cause beta cell failure. Affected beta cells can no longer secrete the expected amount of insulin in response to rising glucose. As a result, blood glucose levels sharply rise, and the diagnosis of diabetes is made. Muscle cells are also at risk, as the buildup of fatty acids inside muscle cells strongly promotes insulin resistance. These fatty acids are stored as intramyocellular lipids (intra = inside, myo = muscles, cellular = cells), or IMCL. Although IMCL is an important energy source for active muscles, an excess can be toxic to cells. Muscle insulin resistance increases the risk for diabetes, while the accumulation of fat in the liver and pancreas triggers beta cell destruction or dysfunction and full-blown diabetes.
Insulin resistance compounds the problem because one of insulin's vital roles is to promote the storage of fat and prevent the breakdown and release of fatty acids from adipocytes. In other words, insulin helps make sure fatty acids stay where they should be. When insulin resistance occurs, insulin can't perform as efficiently and fatty acids are more easily released into the bloodstream, increasing the risk of lipotoxicity. Visceral fat cells are already more insulin resistant than other fat cells, so people with a lot of visceral fat are at higher risk for lipotoxicity.
Insulin resistance compounds the problem because one of insulin's vital roles is to promote the storage of fat and prevent the breakdown and release of fatty acids from adipocytes. In other words, insulin helps make sure fatty acids stay where they should be. When insulin resistance occurs, insulin can't perform as efficiently and fatty acids are more easily released into the bloodstream, increasing the risk of lipotoxicity. Visceral fat cells are already more insulin resistant than other fat cells, so people with a lot of visceral fat are at higher risk for lipotoxicity.
Glucotoxicity
Chronically elevated blood sugar keeps the body constantly awash in a syrupy fluid that sticks to proteins and accumulates on body tissues, interfering with normal cell functions. This process is known as glucotoxicity. The price tag associated with glucotoxicity is steep. It is intrinsically linked to beta cell dysfunction and insulin resistance. Overconsumption of sugars and starches can activate enzymes that speed their conversion to fatty acids and other lipids, such as ceramides, that can be toxic to the liver. Glucotoxicity also damages large blood vessels, leading to diseases such as atherosclerosis (plaque buildup), arteriosclerosis (hardening of the arteries), heart attacks, and strokes. Blood flow to the legs is reduced, resulting in peripheral artery disease, diabetic foot syndrome, and amputations. Muscles begin wasting away due to poor blood flow. This sea of sugar also injures small blood vessels. The lenses of the eyes become less flexible, resulting in retinopathy and poss1ble blindness. The kidneys lose their ability to efficiently filter blood, eventually leading to nephropathy and dialysis. Nerves begin to degenerate, causing neuropathy and decreased sensation, Brain function begins to decline, increasing the risk of dementia and Alzheimer's disease. In men, the blood vessels leading to the penis are damaged, provoking erectile dysfunction. High sugar levels also cripple the immune system cells, which are usually vigilant defenders against viruses and other invaders. Glucotoxicity diminishes their ability to fight infection, and the body's capacity to heal slows to a snail's pace.
Chronically elevated blood sugar keeps the body constantly awash in a syrupy fluid that sticks to proteins and accumulates on body tissues, interfering with normal cell functions. This process is known as glucotoxicity. The price tag associated with glucotoxicity is steep. It is intrinsically linked to beta cell dysfunction and insulin resistance. Overconsumption of sugars and starches can activate enzymes that speed their conversion to fatty acids and other lipids, such as ceramides, that can be toxic to the liver. Glucotoxicity also damages large blood vessels, leading to diseases such as atherosclerosis (plaque buildup), arteriosclerosis (hardening of the arteries), heart attacks, and strokes. Blood flow to the legs is reduced, resulting in peripheral artery disease, diabetic foot syndrome, and amputations. Muscles begin wasting away due to poor blood flow. This sea of sugar also injures small blood vessels. The lenses of the eyes become less flexible, resulting in retinopathy and poss1ble blindness. The kidneys lose their ability to efficiently filter blood, eventually leading to nephropathy and dialysis. Nerves begin to degenerate, causing neuropathy and decreased sensation, Brain function begins to decline, increasing the risk of dementia and Alzheimer's disease. In men, the blood vessels leading to the penis are damaged, provoking erectile dysfunction. High sugar levels also cripple the immune system cells, which are usually vigilant defenders against viruses and other invaders. Glucotoxicity diminishes their ability to fight infection, and the body's capacity to heal slows to a snail's pace.
Dysbiosis
The bacteria, viruses, fungi, and other single-celled organisms harbored by humans are collectively known as microbiota. The largest collection of microbes in the body is found in the gut, although the mouth, skin, and genitals are also common habitats. Each individual is host to between ten and one hundred tril1on symbiotic microbes, containing a mix of communities whose balance has remarkable consequences for health. Some of these organisms promote and protect the host and are commonly referred to as "good bacteria". Those considered "bad bacteria" can harm the host and contribute to various disease processes. A normal, healthy gut is brimming with beneficial bacteria, while less desirable inhabitants are present in smaller numbers. When the balance of bacteria shifts in favor of bad bacteria, the result is a condition known as dysbiosis. Research linking dysbiosis to the epidemic of chronic disease is rapidly mounting. Correlations have been made between dysbiosis and heart disease, cancers, allergic disorders, inflammatory bowel diseases, brain diseases, liver diseases, and, not surprisingly, insulin resistance and diabetes.
Studies suggest that the gut microbiota of individuals with type 2 diabetes are altered in ways that can fuel insulin resistance. Following are some of the key mechanisms of action:
The bacteria, viruses, fungi, and other single-celled organisms harbored by humans are collectively known as microbiota. The largest collection of microbes in the body is found in the gut, although the mouth, skin, and genitals are also common habitats. Each individual is host to between ten and one hundred tril1on symbiotic microbes, containing a mix of communities whose balance has remarkable consequences for health. Some of these organisms promote and protect the host and are commonly referred to as "good bacteria". Those considered "bad bacteria" can harm the host and contribute to various disease processes. A normal, healthy gut is brimming with beneficial bacteria, while less desirable inhabitants are present in smaller numbers. When the balance of bacteria shifts in favor of bad bacteria, the result is a condition known as dysbiosis. Research linking dysbiosis to the epidemic of chronic disease is rapidly mounting. Correlations have been made between dysbiosis and heart disease, cancers, allergic disorders, inflammatory bowel diseases, brain diseases, liver diseases, and, not surprisingly, insulin resistance and diabetes.
Studies suggest that the gut microbiota of individuals with type 2 diabetes are altered in ways that can fuel insulin resistance. Following are some of the key mechanisms of action:
- Increased gut permeability. Dysbiosis increases gut permeability, allowing intact proteins to get into the bloodstream, triggering inflammation and insulin resistance.
- Increased production of pro-inflammatory proteins called cytokines. Cytokines impair insulin sensitivity by causing inflammation and by altering the inner working genes.
- Metabolic endotoxemia. When certain types of bacteria die, their outer cell membranes release toxins that can cross the gut lining and create the inflammatory response associated with insulin resistance. While these toxins (called endotoxins) are present in low concentrations in healthy individuals, amounts can double or triple in obese individuals, resulting in a condition called metabolic endotoxemia.
Why not every Obese Person Develop Insulin Resistance?
You may be wondering how anyone who's very overweight or obese can manage to effectively dodge diabetes. The answer lies in the inherent differences in individual constitutions. Some people have a lot of beta cells and pump out more insulin than other people. Others have very resilient insulin receptors and highly efficient insulin signaling and are protected even when they're overweight or obese. People who manufacture fewer inflammatory cytokines may also be at reduced risk. Individuals with a high tolerance for fatty acids in their liver and pancreas will be afforded protection, While people with a lower tolerance may develop diabetes even it they're only slightly above their ideal weight. Regardless, it's important to realize that anyone who is overweight or obese will experience metabolic malfunctions that increase their risk of chronic diseases, such as heart disease and cancer, even if they don't develop diabetes.
WHY ME?
If you receive a diagnosis of type 2 diabetes, you will no doubt wonder, Why me: You may, unfortunately, be saddled with genes that maximize your risk. Your genes may promote abundant adipose tissue storage. poor insulin production, weak insulin receptor sites, or reduced insulin signaling. However, if genes were the predominant perpetrator, we would expect that type 2 diabetes rates would have been relatively static over the past hundred years. Yet, a hundred years ago, type 2 diabetes was a rare occurrence; today its a raging global epidemic. What scientists have discovered is that when it comes to chronic disease, genes act as a loaded gun. It's almost always diet and lifestyle that pull the trigger. The global culture has become one or overindulgence and underactivity.
The predictable result is a rise in overweight and resistance, prediabetes, and obesity, which dramatically increase the risk of insulin resistance, prediabetes, and type 2 diabetes. How did this happen? Humans are hardwired to be attracted to the tastes of fat, sugar, and salt. Found in low concentrations in nature, these flavors have historically assured us that the food we're about to eat is safe and nourishing. When these substances are concentrated and used as principal ingredients in processed foods, our innate ability to control the appetite becomes unhinged. This is no mere coincidence. Foods that are hyper concentrated in sugar, fat, and salt can, in some circumstances, stimulate pleasure centers in the brain the way that heroin, nicotine, and alcohol do although to a lesser extent. Essentially, they can provide such pleasure that they trigger cravings. To further challenge the senses, portion sizes keep expanding. According to the Centers for Disease Control and Prevention (CDC), the average restaurant meal is four times larger than it was in the 1950s. Not surprisingly, evidence confirms that as portion sizes increase, people eat more. For anyone trying to make a living selling food, addictive flavors and larger portions mean return customers and rising sales.
To add insult to injury, the level of physical activity in today's world has dwindled dramatically since the 1950s. Every possible convenience has been developed to help reduce energy expenditure. Even if people wanted to increase their activity, many neighborhoods lack sidewalks and safe places for exercise.
It's little wonder that in the United States and all other countries that adapt their lifestyle, being overweight or obese is now the new normal, with over 70 percent of the population being affected. In this environment, staying slim seems a greater mystery than becoming overweight or obese. The good news is that this dark cloud has a silver lining. By carefully controlling your environment (that is, your diet and lifestyle), you can change the expression of your genes, essentially taking your flinger off the trigger.
If you receive a diagnosis of type 2 diabetes, you will no doubt wonder, Why me: You may, unfortunately, be saddled with genes that maximize your risk. Your genes may promote abundant adipose tissue storage. poor insulin production, weak insulin receptor sites, or reduced insulin signaling. However, if genes were the predominant perpetrator, we would expect that type 2 diabetes rates would have been relatively static over the past hundred years. Yet, a hundred years ago, type 2 diabetes was a rare occurrence; today its a raging global epidemic. What scientists have discovered is that when it comes to chronic disease, genes act as a loaded gun. It's almost always diet and lifestyle that pull the trigger. The global culture has become one or overindulgence and underactivity.
The predictable result is a rise in overweight and resistance, prediabetes, and obesity, which dramatically increase the risk of insulin resistance, prediabetes, and type 2 diabetes. How did this happen? Humans are hardwired to be attracted to the tastes of fat, sugar, and salt. Found in low concentrations in nature, these flavors have historically assured us that the food we're about to eat is safe and nourishing. When these substances are concentrated and used as principal ingredients in processed foods, our innate ability to control the appetite becomes unhinged. This is no mere coincidence. Foods that are hyper concentrated in sugar, fat, and salt can, in some circumstances, stimulate pleasure centers in the brain the way that heroin, nicotine, and alcohol do although to a lesser extent. Essentially, they can provide such pleasure that they trigger cravings. To further challenge the senses, portion sizes keep expanding. According to the Centers for Disease Control and Prevention (CDC), the average restaurant meal is four times larger than it was in the 1950s. Not surprisingly, evidence confirms that as portion sizes increase, people eat more. For anyone trying to make a living selling food, addictive flavors and larger portions mean return customers and rising sales.
To add insult to injury, the level of physical activity in today's world has dwindled dramatically since the 1950s. Every possible convenience has been developed to help reduce energy expenditure. Even if people wanted to increase their activity, many neighborhoods lack sidewalks and safe places for exercise.
It's little wonder that in the United States and all other countries that adapt their lifestyle, being overweight or obese is now the new normal, with over 70 percent of the population being affected. In this environment, staying slim seems a greater mystery than becoming overweight or obese. The good news is that this dark cloud has a silver lining. By carefully controlling your environment (that is, your diet and lifestyle), you can change the expression of your genes, essentially taking your flinger off the trigger.
Article & Video Review
|
|
|