Welcome!
Congratulations on starting your Basic Culinary Medicine Course. You’ve taken the first step in taking control of your health by starting in your kitchen. Before you get started, we will have a brief overview of the course.
The goal of the CulinaryMD is to get you cooking and eating mostly a whole-food plant-based diet and preparing them the CulinaryMD way. We want to help you become more comfortable first in your home kitchen and better understand the evidence-based utilization of the whole food plant-based diet to prevent, treat, and even reverse some chronic disease. You can achieve these objectives by developing basic culinary skills blended with the science of medicine.
As a part of the CulinaryMD community of learners, we expect you to engage with instructors by sharing your experiences and asking questions using the provided help icon. The CulinaryMD team is looking forward to helping you navigate and experience the vast world of healthy cooking alongside health education. We anticipate that you prepare to learn, experience, and be open to challenges.
Good luck with your course! and Happy learning!
Your CulinaryMD Team
Congratulations on starting your Basic Culinary Medicine Course. You’ve taken the first step in taking control of your health by starting in your kitchen. Before you get started, we will have a brief overview of the course.
The goal of the CulinaryMD is to get you cooking and eating mostly a whole-food plant-based diet and preparing them the CulinaryMD way. We want to help you become more comfortable first in your home kitchen and better understand the evidence-based utilization of the whole food plant-based diet to prevent, treat, and even reverse some chronic disease. You can achieve these objectives by developing basic culinary skills blended with the science of medicine.
As a part of the CulinaryMD community of learners, we expect you to engage with instructors by sharing your experiences and asking questions using the provided help icon. The CulinaryMD team is looking forward to helping you navigate and experience the vast world of healthy cooking alongside health education. We anticipate that you prepare to learn, experience, and be open to challenges.
Good luck with your course! and Happy learning!
Your CulinaryMD Team
What is Culinary Medicine?
Culinary medicine (CM) is a fast emerging, evidence-based field that blends nutrition education with culinary knowledge and skills to help patients maintain health, prevent, and manage food-related diseases by having healthy food choices in conjunction with appropriate medical care. Diet has been identified as the most crucial risk factor for morbidity and mortality worldwide and is associated with over 11 million deaths annually. Despite the horrifying statistics, most health care providers fail to receive the recommended number of hours studying nutrition in medical training. The majority of nutrition education offered in medical and interprofessional curriculum includes didactics mostly focused on the biochemistry of nutrients and deficiency states. There has been a limited emphasis on the risk of overnutrition that is far more significant due to high intake of calorie-dense, ultra-processed foods. CM fills this identified educational gap by focusing on nutrition knowledge, practical dietary behavior changes, and cooking skills needed to prepare delicious, healthy, and accessible food. Consideration of time availability, financial resources, and cultural food traditions is also essential for any successful CM program.In the recent years, understanding the importance of the CM approach to nutrition education in health professional training programs (HPTPs) has increased. However, the lack of an easily accessible, evidence-based guide to implementing CM has constituted a significant barrier at most institutions. The Culinary Medicine Curriculum (CMC), published in collaboration with the American College of Lifestyle Medicine in December 2019, is the first comprehensive, open-source guide created to support the implementation of CM at academic institutions worldwide.
After the successful CM elective course for medical and physician assistant students at Stanford University School of Medicine, the CMC is modeled. Both the Stanford CM course and the CMC were developed by a group of experts whose training includes internal medicine, family medicine, pediatrics, obesity medicine, lipidology, integrative medicine, lifestyle medicine, nutrition science, epidemiology, public policy, medical school curriculum design, and culinary arts.
The Stanford CM course was taught by dually trained physician-chefs with nutrition expertise that this combination of expertise. With the identified limitations, the CMC was adapted to enable a wide variety of health professionals to teach CM in their training programs. Examples of combinations of instructors likely to be successful in teaching a CM course using the CMC include (a) a professional with training in culinary arts, nutrition; (b) a clinician-educator who is knowledgeable about nutrition and cooking; or (c) 2 or more instructors trained in lifestyle medicine fields that cover formal or informal culinary training, nutrition expertise, and direct patient care experience.
The CMC incorporates lessons learned in medical practice caring for diverse patients of all ages and varying education and resource levels. Key goals of the curriculum include presenting healthy food as delicious, simple, filling, and inexpensive; translating lessons learned to healthy eating on-the-go; practicing motivational interviewing on healthy dietary behavior changes.
After the successful CM elective course for medical and physician assistant students at Stanford University School of Medicine, the CMC is modeled. Both the Stanford CM course and the CMC were developed by a group of experts whose training includes internal medicine, family medicine, pediatrics, obesity medicine, lipidology, integrative medicine, lifestyle medicine, nutrition science, epidemiology, public policy, medical school curriculum design, and culinary arts.
The Stanford CM course was taught by dually trained physician-chefs with nutrition expertise that this combination of expertise. With the identified limitations, the CMC was adapted to enable a wide variety of health professionals to teach CM in their training programs. Examples of combinations of instructors likely to be successful in teaching a CM course using the CMC include (a) a professional with training in culinary arts, nutrition; (b) a clinician-educator who is knowledgeable about nutrition and cooking; or (c) 2 or more instructors trained in lifestyle medicine fields that cover formal or informal culinary training, nutrition expertise, and direct patient care experience.
The CMC incorporates lessons learned in medical practice caring for diverse patients of all ages and varying education and resource levels. Key goals of the curriculum include presenting healthy food as delicious, simple, filling, and inexpensive; translating lessons learned to healthy eating on-the-go; practicing motivational interviewing on healthy dietary behavior changes.
The Science of Culinary Nutrition
NUTRITION PRESCRIPTION
|
Nutrition prescription is one of the Core Lifestyle Medicine Competencies. Dr. Dennis Burkitt emphasized the significant dietary changes that followed the Industrial Revolution, causing the major increase of chronic disease incidence and prevalence whenever there is a reduction in starch foods and fiber intake and a tremendous increase in animal fats, salt, and salt, and sugar.
|
One study published in the International Journal of Epidemiology revealed a strong correlation between serum cholesterol, diet, and coronary heart disease. People in this specific part of the world have no exposure to a Western diet. It's surprising that heart disease, the number one killer among Americans, is almost non-existent in Uganda's African population. The staple foods, green plantain, and steamed sweet potatoes in banana leaves: cassava, yams, and millet are also staple commodities, particularly of the non-Baganda groups, while all take pumpkins, tomatoes, and green leafy vegetables. The adequacy of protein in the diet depends almost entirely on how they consume groundnuts and cereals (O'Keefe, 2019).
|
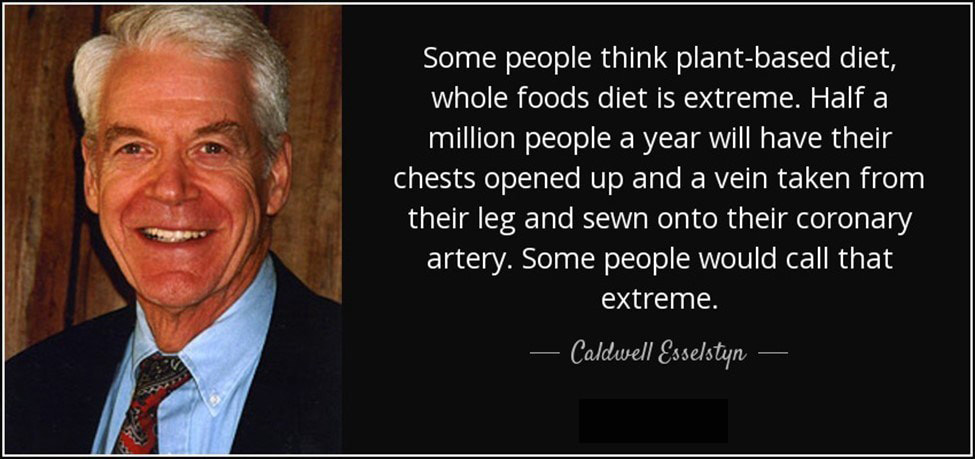
Dr. Caldwell Esselstyn also noted that coronary artery disease is virtually absent in cultures that eat plant-based diets, such as the Tarahumara Indians of northern Mexico and Papua highlanders of New Guinea, and the inhabitants of rural China and central Africa. Hundreds of thousands of rural Chinese live for years without a single documented myocardial infarction (Esselstyn, 2017).
|
|
The former editor-in-chief of the American Journal of Cardiology, Dr. William Roberts, is convinced that the disease has a single cause, namely cholesterol and that the other so-called atherosclerotic risk factors are only contributory at most. In other words, if the total serum cholesterol is 90 to 140mg/dL, there is no evidence that cigarette smoking, systemic hypertension, diabetes mellitus, inactivity, or obesity produces atherosclerotic plaques. Hypercholesterolemia is the only direct atherosclerotic risk factor; the others are indirect. Dr. Roberts also implied that the goal for all populations – not just those with heart attacks or strokes, diabetes mellitus, or non-coronary atherosclerotic events – must be LDL cholesterol <100 mg/dL and ideally <70mg/dL. If such a goal was created, the great scourge of the Western world would be eliminated. In fact, it was published in the Journal of Lipid Research that the average blood cholesterol level in the United States (and other countries using Western medicine guidelines), the so-called normal level (up to 200mg/dL), was actually abnormal. It was accelerating atherogenesis and putting a large fraction of the so-called normal population at a higher risk for coronary heart disease.
|
It was also found out that almost 75% of heart attack patients fell within recommended targets for LDL cholesterol demonstrating that the current guidelines may not be low enough to cut heart attack risk. Accumulating data from multiple lines of evidence consistently demonstrate that the physiologically normal LDL level and the thresholds for atherosclerosis development and coronary heart disease events are approximately 50 to 70 mg/dL (O'Keefe, et al, 2004).
The well-known Longitudinal Study of Aging Danish Twins, research on genetics and longevity suggested that genetics account only for 20% to 30% of life span, with the rest due to environmental and lifestyle factors (McGue, Christensen, 2007). With these findings, Dan Buettner, a journalist, set out a remarkable work of finding the longest-lived people on earth and called them the “Blue Zone.” They are across the globe with a diverse history, genetics, cultures, traditions, and environments. But they have many things in common, including eating a whole foods diet with an average of 90% calories coming from plant-based sources and an active lifestyle. In 2004, Dan Buettner teamed up with National Geographic, and the world’s best longevity researchers began their exploration and were able to identify 5 Blue Zones (Blue Zones, n.d.).
|
The first Blue Zone identified by Buettner was Sardinia, Italy. There have always been centenarians in Sardinia, but in the most mountainous inland region called Barbagia with nearly 58,000 population, a cluster of villages in the island is linked to exceptional longevity. This is due to geographic isolation and the undiluted genes of the residents. But even more importantly, Sardinians of this area are culturally isolated and very traditional.
|
They have kept their healthy lifestyle throughout generations; they still hunt, fish, and harvest the food they eat. Sardinians are farmers and shepherds, and they live in a clean environment. They remain close with friends and family throughout their lives (Blue Zones, n.d.).
|
Ikaria, Greece, is another Blue Zone, a relatively remote island with only a little more than eight thousand inhabitants. It’s in the Aegean Island that is found to be one of the world’s lowest rates of middle-age mortality and the lowest rates of dementia. Ikarians exercised mindlessly. They eat a variation of the Mediterranean diet, with lots of fruits and vegetables, whole grains, beans, potatoes, and olive oil.
|
They enjoy drinking antioxidant-rich herbal teas coming from wild rosemary, sage, and oregano that also act as a diuretic that maintains blood pressure. People in Ikaria doesn’t mind time and lives with a relaxed lifestyle (Blue Zones, n.d.).
|
Okinawa, Japan, is another Blue Zone with a unique outlook on life. They’re capable of letting difficult early years remain in the past while they are enjoying today’s simple pleasures. Okinawans have one of the highest ratios of centenarians, about 6.5 in 10,000 live to be 100 lower rates of disease than Americans in every given category.
|
Their staple food is composed of vegetables, sweet potatoes (67%) with high nutrients and low in calories. The Okinawan diet is rich in foods made with soy, like tofu and miso soup. They also have medicinal herbs including ginger and turmeric in their regular food consumption. (Blue Zones, n.d.).
|
Another Blue Zone is Costa Rica’s hilly Nicoya region. The mestizos (people combined European and American Indian descent) reach the age of ninety at two and one-half times the rate of northern Americans and have much less cancer, heart disease, and diabetes. The Caribbean nation is economically secure and has excellent health care, and Nicoyans have also stayed relatively free of the diseases of affluence that afflict Costa Rica’s city-dwelling populations.
|
Nicoyan centenarians frequently visit with neighbors, and they tend to live with families and children or grandchildren who provide support, as well as a sense of purpose. One unique tradition of Nicoyans is eating a light dinner early in the evening. For most of their lives, Nicoyan centenarians ate their staple diet composed of squash, corn, and beans.
And the last Blue Zone we will discuss is a unique religious group that is called the healthiest people in the world, the Seventh Day Adventists in Loma Linda, California. Unlike the four identified Blue zones, this religious group is not in an isolated place in the United States. Loma Linda is in Southwestern San Bernardino County (Blue Zones, n.d.).
|
HEALTHIEST PEOPLE IN THE WORLD
In the 1970’s and ‘80s the first Adventist study was conducted in Loma Linda California with more than thirty-four thousand people who were followed for fourteen long years. It is uncommon in epidemiological studies that researchers can survey a group of people with very similar lifestyles and practices. |
And most importantly many distinct dietary subgroups, enabling them to more effectively isolate the impact of diet on health. The Seventh-day Adventist is a religious group established in the mid-ninteenth century.
The counsels of Seventh-day Adventists are largely inspired by the biblical verse Genesis 1:29: “And God said, Behold, I have given you every herb bearing seed, which is upon the face of all the earth, and every tree, in which is the fruit of a tree yielding seed; to you it shall be for meat.” In other words, eat real food, eat plants. They also have comprehensive guide and counsels written in many books emphasizing healthy lifestyle as part of their doctrine and beliefs.
The counsels of Seventh-day Adventists are largely inspired by the biblical verse Genesis 1:29: “And God said, Behold, I have given you every herb bearing seed, which is upon the face of all the earth, and every tree, in which is the fruit of a tree yielding seed; to you it shall be for meat.” In other words, eat real food, eat plants. They also have comprehensive guide and counsels written in many books emphasizing healthy lifestyle as part of their doctrine and beliefs.
|
The Seventh-day Adventist church view health as central to their faith and that made them one of the most interesting groups to study, from the perspective of diet. They have such a similar overall lifestyle. Active members of the church are not smokers or alcohol consumers, they have a strong religious faith and community, and they exercise regularly.
|
The Adventists’ staple diet was largely composed of fruits and vegetables, nuts, legumes, and soy foods. Although other Seventh-day Adventists are consuming animal products, they still avoid certain types of foods they considered unclean based on a Biblical and health perspective. Specific members also follow a different vegetarian pattern, including vegan to Lacto-Ovo vegetarian, to pesco-vegetarian (Banta et al, 2018).
In 2002 a second major Adventist study was started, led by Dr. Gary Fraser and a team of researchers from Loma Linda University, which included ninety-six thousand participants from across the United States and Canada. The results from that study showed that Adventist meat-eaters had the biggest waistlines and had a higher death rate than their vegetarian Adventist counterparts. They also tended to have worse overall dietary habits, including greater consumption of highly processed foods such as sugar, soda, and refined grains. This raises the question of whether it was the animal foods or the processed food, or both that led to shorter lives in this cohort. Although we cannot tease that out with this study, what we can tell is that the lacto-ovo vegetarians, the pesco-vegetarians, and the vegans all had significantly lower mortality rates compared to the meat-eaters.
It’s worth noting that even those Adventists classified as meat-eaters were much less so than most Americans. The meat-eating Adventists’ diet (in terms of daily intake in grams) was largely composed of fruits and vegetables, nuts, legumes, and soy foods. And the overall better life expectancy of the community reflects that fact.
The Adventists are one of the most interesting groups to study, from the perspective of diet, because they have such a similar overall lifestyle. It is rare in epidemiological studies that researchers can observe a group of people with very similar lifestyles but so many distinct dietary subgroups, enabling them to more effectively isolate the impact of diet on health.
The Adventists are one of the most interesting groups to study, from the perspective of diet, because they have such a similar overall lifestyle. It is rare in epidemiological studies that researchers can observe a group of people with very similar lifestyles but so many distinct dietary subgroups, enabling them to more effectively isolate the impact of diet on health.
When it comes to America’s leading cause of death – heart disease and cancer – the vegetarian Adventist, again, fairly well. They have the lowest rate of heart disease in the nation. In men, the risk of fatal heart disease was “significantly related to beef intake.” The risk of colon cancer was increased by 88% in Adventists who ate meat over their vegetarian counterparts. Diabetes, our rapidly growing national epidemic, is rare among the Adventists. Indeed, they boast the nation’s lowest rates of the disease. Switching to plant-based nutrition involves a radical remaking of what’s on the plate and in the pantry. It means changing a lifetime of habits, learning new skills, and developing new tastes. Some people do best with a slow, step-by-step transition, while others choose to go all in, all at once (Adventist Health Studies, 2008).
THE CLINICAL PIONEERS OF PLANT-BASED NUTRITION
In the late 1950s, a young man named Nathan Pritikin had been diagnosed with heart disease at just forty-two years of age. Through long experimentation with diet, he eventually reversed his disease. In 1975, he opened up a “longevity center” in California to share his regimen, which was essentially whole foods, primarily plant-based diet, along with exercise every day. Pritikin’s patients got better – a lot better! Risk factors for heart disease improved across the board, cholesterol went down, and arterial function and blood flow improved, along with a host of other health transformations. Pritikin’s works attracted a great deal of attention in his day, but without medical credentials or controlled trials, he was never fully accepted by the establishment. Since his death, more than 100 studies in peer-reviewed journals have validated the program’s effectiveness. Meanwhile, however, the task of scientifically demonstrating that diet and lifestyle change could reverse heart disease was being taken up by an independent-minded young physician from the Lone Star State (Li & Heber, 2020).
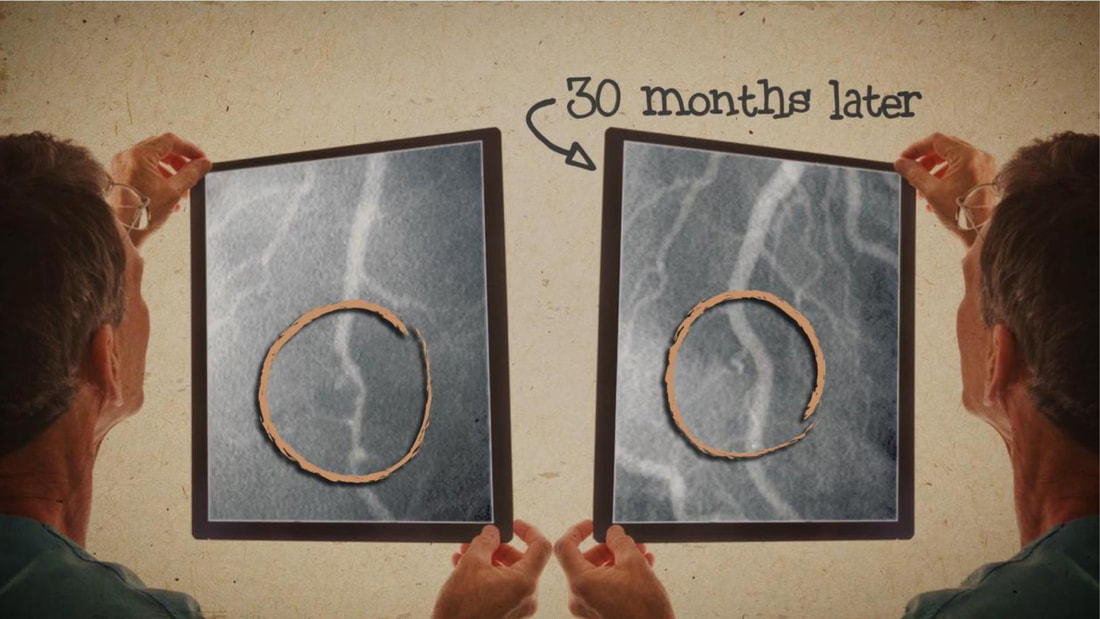
After only twenty-four months, the patients who made comprehensive lifestyle changes showed improvement (reversal) in their heart disease, whereas those in the randomized control group got worse. This, the first randomized controlled trial showing that lifestyle changes alone could reverse heart disease, was published in the Journal of the American Medical Association. In 1984, he launched the Lifestyle Heart Trial (Ornish et al, 1998).
|
In the Cleveland Clinic, Dr. Caldwell Essenstyn was also developing a study. He had encountered some resistance from the establishment. Most senior cardiologists at the Cleveland Clinic, he writes, “did not believe there was a connection between diet and coronary disease. Nevertheless, in 1985, the Department of Cardiology agreed to participate in his first proposed study.
|
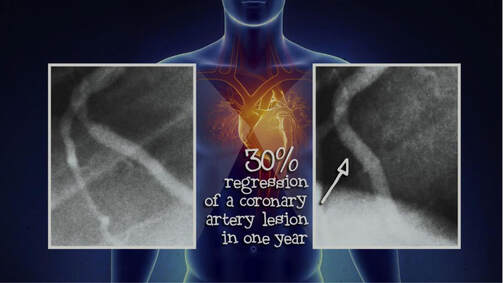
It would refer patients to him – primarily those for whom bypass surgery or angioplasty had failed, and several who had been told there was nothing more that could be done for them. Esselstyn’s hypothesis was that plant-based nutrition could reduce their cholesterol levels below 150 mg/dL (closer to the level seen in those traditional cultures that had no heart disease) and, in so doing, slow or halt the disease process. By 1988 a cohort of twenty-four people with severe, progressive coronary artery disease was eating a very low-fat, plant-based diet under his supervision (Esselstyn, 2017).
|
|
|
From a dietary standpoint, Ornish’s and Esselstyn’s studies were very similar. However, unlike Esselstyn, who instructed patients to continue their medications, Ornish did not use cholesterol-lowering medications in his study. Moreover, he stipulated other lifestyle changes in addition to the nutritional component, including relaxation techniques, moderate exercise, smoking cessation, and participation in a support group – interventions he believes are also critical to the success of the program. His study included forty-eight patients who were randomized into two groups: twenty-eight of patients made the recommended diet and lifestyle changes, while the other twenty served as a control group, following standard medical treatment and dietary advice from the American Heart Association.
Ornish’s work was the first to be made public. In 1990 he published the one-year results. Most of the experimental group reported a complete or nearly complete disappearance of chest pains. But patients not only felt better, they were better. When measurements were taken of their narrowed arteries using angiograms, 82% showed an increased diameter (reversal). Only one patient who had poor adherence showed significant progression (worsening).
In 2006, Esselstyn launched a second, larger study, this time following 198 patients who adopted his plant-based nutritional program. In 2014 he published the results: of those who complied with the diet, 93% experienced an improvement in angina symptoms. And only one patient experienced a major cardiovascular event due to recurrent disease (a stroke) – demonstrating that his diet was protective for 99.4% of patients who followed it. In comparison, among the twenty-one participants who did not adhere to the program, thirteen experienced further cardiac events, including two deaths.
Ornish’s and Esselstyn’s studies represent a dramatic medical breakthrough. Until that point, the best that drugs and surgical treatments could do was manage heart disease. They ended up doing something few even believed was possible: they showed that heart disease is reversible. And they did it with lifestyle interventions that had no adverse side effects. By merely stopping eating foods that were clogging up their arteries and instead eating a healthy plant-based diet, their patients began to heal – at any age. Their remarkable turnarounds show that it’s never too late when it comes to heart disease.
VEGAN IS NOT ALWAYS HEALTHY
|
|
It’s important to understand that one can adopt a vegan or vegetarian diet (perhaps for ethical reasons) and still end up eating very unhealthy foods. Merely avoiding animal foods is not the answer to good health. Studies have shown that vegetarians have a decreased risk of cancer, less obesity, and, depending on the task you look at, possibly greater longevity.
|
Those studies track the reduced consumption of unhealthy animal products and increase healthy plant-based foods in the diet – greater consumption of fruits and vegetables, whole grains, beans, and other legumes, with all their corresponding beneficial nutrients micronutrients.
In the extensive European Prospective Investigation into Cancer and Nutrition (or EPIC) study, four combined lifestyle behaviors were associated with an extra fourteen years of longevity – not smoking, only moderate consumption of alcohol, physical activity, and the consumption of at least five servings of fruits and vegetables every day (Boeing, 2017).
Becoming a vegetarian should never be considered a ticker to health all by itself. Doughnuts, French fries, and banana splits are all vegetarian, and not one of them will make a top-ten health food list any time soon. A whole-food, plant-based diet stays away from refined grains, highly processed carbohydrates and sugars, and oils. Like the aforementioned EPIC study, there have even been studies that did not find a significant difference in the life expectancy between meat-eaters and vegetarians. But here’s a key to interpreting that data: the vegetarians in the EPIC study were eating only half the fiber of the Adventist vegetarians in Loma Linda. That means they were eating far fewer whole plant foods! The Loma Linda vegetarians were eating many more whole foods and plants and all the healthy fiber and nutrients they are packed in. The results speak for themselves – an ordinary population, genetically diverse, with extraordinary health outcomes. As Garth Davis, MD, puts it, “If everyone ate like a Seventh-day Adventist, everyone would have the health of a Seventh-day Adventist.”
In the extensive European Prospective Investigation into Cancer and Nutrition (or EPIC) study, four combined lifestyle behaviors were associated with an extra fourteen years of longevity – not smoking, only moderate consumption of alcohol, physical activity, and the consumption of at least five servings of fruits and vegetables every day (Boeing, 2017).
Becoming a vegetarian should never be considered a ticker to health all by itself. Doughnuts, French fries, and banana splits are all vegetarian, and not one of them will make a top-ten health food list any time soon. A whole-food, plant-based diet stays away from refined grains, highly processed carbohydrates and sugars, and oils. Like the aforementioned EPIC study, there have even been studies that did not find a significant difference in the life expectancy between meat-eaters and vegetarians. But here’s a key to interpreting that data: the vegetarians in the EPIC study were eating only half the fiber of the Adventist vegetarians in Loma Linda. That means they were eating far fewer whole plant foods! The Loma Linda vegetarians were eating many more whole foods and plants and all the healthy fiber and nutrients they are packed in. The results speak for themselves – an ordinary population, genetically diverse, with extraordinary health outcomes. As Garth Davis, MD, puts it, “If everyone ate like a Seventh-day Adventist, everyone would have the health of a Seventh-day Adventist.”
|
One person who certainly appears to have the health of a Seventh-day Adventist – or of the rural Chinese he studied – is T. Colin Campbell. Today, in his eighties and still robust and active, he runs a nutritional center, teaches at Cornell, and lectures around the world on the benefits of the whole foods, plant-based diet.
|
WHAT FOLLOWS AFTER THE SWALLOWS?
Have you ever thought of “What follows after the swallows?” Well, typically, we only start to recall the kind of food we ate when something goes wrong. We would try to remember our food diary when our blood sugar went up or signs of high blood pressure, mostly when we have stomach upset or allergies. Most people would commonly attribute some of their discomforts to the food groups they ate. One best example is high meat and crustacean intake. This food intake is commonly followed by the increased uric acid build-up in response to its exceedingly high purine content causing stiffness, pain, and even swelling of joints, commonly affecting the digits and ankles in less than twenty-four hours after ingestion.
Very few are interested in carefully reading food labels, ingredients used, and the nutritional descriptions before buying them from the market and finally end up on our table for routine daily consumption. There seems to be a need for individuals to understand how food is processed and where everything goes after swallowing. Perhaps it is a must for everyone to effectively equip ourselves with basic knowledge on the digestion, absorption, elimination, and some biochemical processes in the body. After all, EATING is the most enjoyable necessity that everyone has, and everyone does.
We have to emphasize how food is prepared, processed, and combined before it reaches our table. Every alteration we make changes the quality and quantity of substances that we may get from food. Is it the high temperature that has something to do with the degradation of vitamins, minerals, enzymes, and other active substances like antioxidants? Or could it be the cutting, pressing, blending, or grinding? We may also be confused about the conflicting principles of which varieties are safe to combine or taken first before another to maximize absorption. And how about the oxidative stress from each meal and what it does to our DNA? And even more interesting is the DYSBIOSIS that happens in the gut, which can be a potential cause of several events in developing the chronic disease.
DIGESTION, ABSORPTION, METABOLISM, and EXCRETION
Among all the organ systems that the human body has, the Digestive system is one of the busiest systems that seem to be working so hard than we thought. Anyone exposed to a certain stimulus, a very enticing smell of crispy fried chicken, for example, would already send the signal to the brain to send the command and prompt the digestive system to work. That single smell has many messages to convey into the human body, and you appreciate the response almost immediately. We should start learning the basics of digestion, which the body does from sunrise to sunset.
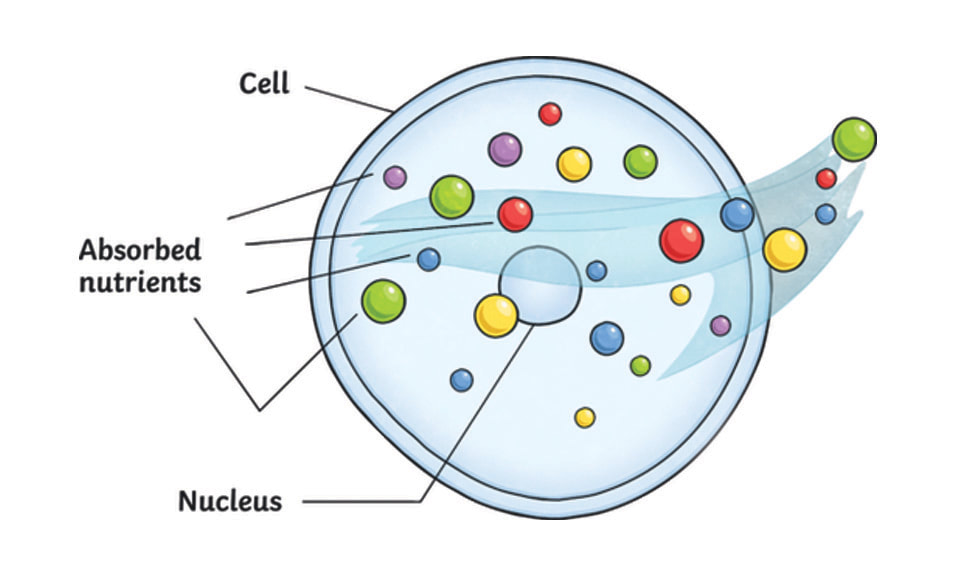
People are now getting a larger grasp of food significance and eating more responsibly. Food supplies the necessary nutrients to sustain every part of the human body for energy, maintenance, and growth. Each food particles are composed of complex substances broken down to simpler forms that the cells can use.
Among all the organ systems that the human body has, the Digestive system is one of the busiest systems that seem to be working so hard than we thought. Anyone exposed to a certain stimulus, a very enticing smell of crispy fried chicken, for example, would already send the signal to the brain to send the command and prompt the digestive system to work. That single smell has many messages to convey into the human body, and you appreciate the response almost immediately. We should start learning the basics of digestion, which the body does from sunrise to sunset.
People are now getting a larger grasp of food significance and eating more responsibly. Food supplies the necessary nutrients to sustain every part of the human body for energy, maintenance, and growth. Each food particles are composed of complex substances broken down to simpler forms that the cells can use.
|
We should never forget that the CELL is the ultimate destination of the nutrients found in food. It would undergo many tedious courses of action, including digestion, absorption, and metabolism that are the three interrelated processes that act on food in many different levels to prepare it for use by the body. The last process is excretion, where the elimination of undigestible or unusable substances takes place.
|
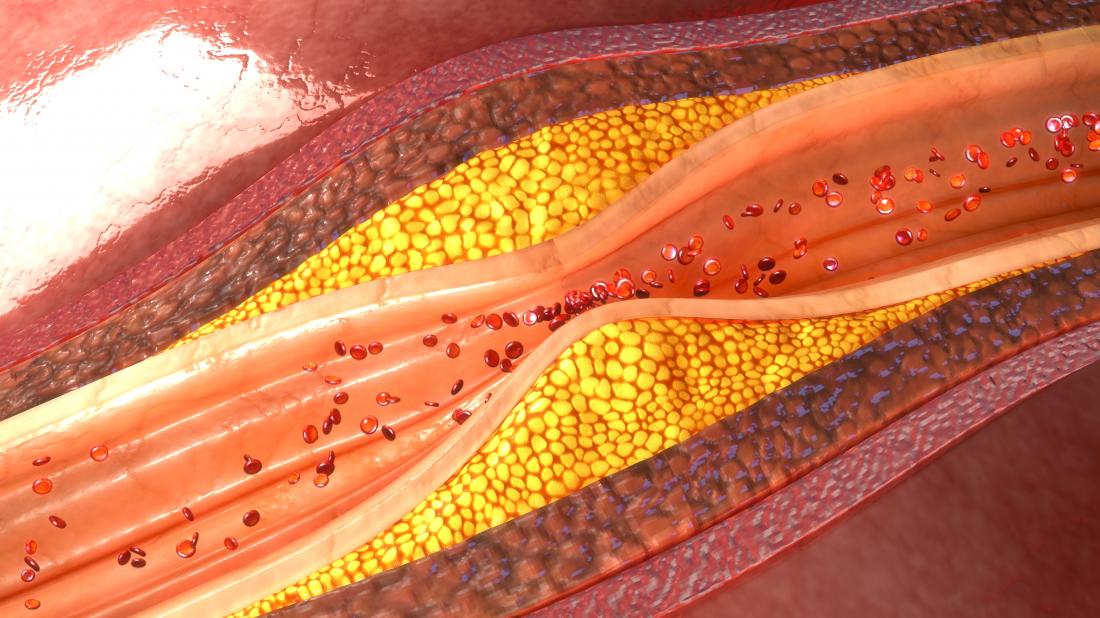
Among the many processes and chemical interactions happening in the human body, FOOD contributes one of the most extensive roles. We have to remember that anything we put inside our mouth may eventually end up in our blood vessels and carried out to trillions of cells for utilization. So whether we ate the healthy stuff, the greases, or the toxins, they may all ooze down to the blood for cell uptake, and there’s no way to take them back out of the system.
Digestion is the First step in preparing food for use by the cells. It is the process by which food is mechanically broken down into smaller particles along the gastrointestinal tract stretch. These end products of digestion would move from the gastrointestinal tract into the blood or lymphatic system, a process called absorption.
Digestion is the First step in preparing food for use by the cells. It is the process by which food is mechanically broken down into smaller particles along the gastrointestinal tract stretch. These end products of digestion would move from the gastrointestinal tract into the blood or lymphatic system, a process called absorption.
Digestion takes place in the alimentary canal and the accessory organs. The alimentary canal is a long, hollow, muscular tube that extends through the body from the mouth and ends at the anus. It includes the oral cavity, pharynx, esophagus, stomach, small intestine, and large intestine. The muscle rings, called sphincters, are structures that separate segments of the alimentary canal. They act as valves to control the passage of food. When the muscles contract, the passageway closes; when the muscles relax, the passageway opens.
THE MOUTH
Mechanical and chemical digestion occurs simultaneously throughout the alimentary canal. It starts by effective mastication (chewing) of food in the mouth. Food is initially broken down into smaller forms while enzymes are secreted by the salivary glands to mix with the food. Chewing serves to grind food into smaller pieces and increase the surface area upon which digestive enzymes can work. The larger surface area facilitates digestion, because virtually all digestive activities are driven by enzymatic reactions. In addition, saliva is released in the mouth. Saliva helps to moisten food, which allows for easier swallowing. Although food could be completely digested without first entering the mouth, gastrointestinal transit time is reducing when food is thoroughly masticated prior to swallowing. Mechanical digestion is the physical breaking down of food into smaller pieces. Chemical digestion involves the splitting of complex molecules into smaller forms.
Mechanical and chemical digestion occurs simultaneously throughout the alimentary canal. It starts by effective mastication (chewing) of food in the mouth. Food is initially broken down into smaller forms while enzymes are secreted by the salivary glands to mix with the food. Chewing serves to grind food into smaller pieces and increase the surface area upon which digestive enzymes can work. The larger surface area facilitates digestion, because virtually all digestive activities are driven by enzymatic reactions. In addition, saliva is released in the mouth. Saliva helps to moisten food, which allows for easier swallowing. Although food could be completely digested without first entering the mouth, gastrointestinal transit time is reducing when food is thoroughly masticated prior to swallowing. Mechanical digestion is the physical breaking down of food into smaller pieces. Chemical digestion involves the splitting of complex molecules into smaller forms.
THE ESOPHAGUS
Once food is swallowed it leaves the mouth and travels to the stomach through a pipe of about 10- inch in length called the esophagus. While gravity helps, the food travel down to the alimentary canal through the movement of the gut smooth muscles called peristalsis. Peristaltic contractions continually push food forward along the digestive tract. Reverse peristalsis, or vomiting, is the violent contractions of the stomach and esophagus in the opposite direction.
THE STOMACH
Next to the esophagus is the stomach. It is a structure that functions as holding reservoir that churns food and secretes digestive juices containing acids and enzymes through the lining mucosa. Generally, gastric emptying is approximately two to four hours. This means, food stays in the stomach for a while before it goes down to the small intestine. A number of factors can affect the gastric emptying time; for example, liquids leave the stomach faster than solids. Fats stays longer than protein, and carbohydrates exit faster than protein. High-fiber carbohydrates (sweet potato and whole grains) stay in the digestive tract longer than simple carbohydrates (cakes and pastries). And this plays an important role in determining the glycemic index, the relative ranking of carbohydrate in foods according to how they affect blood glucose levels.
Once food is swallowed it leaves the mouth and travels to the stomach through a pipe of about 10- inch in length called the esophagus. While gravity helps, the food travel down to the alimentary canal through the movement of the gut smooth muscles called peristalsis. Peristaltic contractions continually push food forward along the digestive tract. Reverse peristalsis, or vomiting, is the violent contractions of the stomach and esophagus in the opposite direction.
THE STOMACH
Next to the esophagus is the stomach. It is a structure that functions as holding reservoir that churns food and secretes digestive juices containing acids and enzymes through the lining mucosa. Generally, gastric emptying is approximately two to four hours. This means, food stays in the stomach for a while before it goes down to the small intestine. A number of factors can affect the gastric emptying time; for example, liquids leave the stomach faster than solids. Fats stays longer than protein, and carbohydrates exit faster than protein. High-fiber carbohydrates (sweet potato and whole grains) stay in the digestive tract longer than simple carbohydrates (cakes and pastries). And this plays an important role in determining the glycemic index, the relative ranking of carbohydrate in foods according to how they affect blood glucose levels.
THE SMALL INTESTINE
After churning of food in the stomach, the end product called “chyme” is then transported to the small intestine which is the primary site of digestion and absorption of nutrients into the body. In this part of the alimentary canal, a lot of enzymes are secreted that helps break apart larger molecules into particles small enough to cross the intestinal cell wall into the bloodstream. Chyme typically remains in the small intestine for 3-10 hours, depending on its nutrient composition. Like in gastric emptying, fat takes the longest to digest and so it stays in the small intestine for quite a while. There are folds found in the small intestine called villi and microvilli that significantly increase the surface area to approximately 600 times that of a simple cylinder.
Each day, the small intestine receives between one and three gallons (or six to twelve liters) of this liquid. The small intestine carries out most of the digestive process, absorbing almost all of the nutrients we can get from foods into the bloodstream.
After churning of food in the stomach, the end product called “chyme” is then transported to the small intestine which is the primary site of digestion and absorption of nutrients into the body. In this part of the alimentary canal, a lot of enzymes are secreted that helps break apart larger molecules into particles small enough to cross the intestinal cell wall into the bloodstream. Chyme typically remains in the small intestine for 3-10 hours, depending on its nutrient composition. Like in gastric emptying, fat takes the longest to digest and so it stays in the small intestine for quite a while. There are folds found in the small intestine called villi and microvilli that significantly increase the surface area to approximately 600 times that of a simple cylinder.
Each day, the small intestine receives between one and three gallons (or six to twelve liters) of this liquid. The small intestine carries out most of the digestive process, absorbing almost all of the nutrients we can get from foods into the bloodstream.
Looking at the small intestine as a pipe, it seems hard to believe that an organ so narrow could do such a big job. However, looks can be deceiving. The absorptive surface area of the small intestine is actually about 250 square meters (almost 2,700 square feet) – the size of a tennis court! How is this possible? The small intestine has three features which allow it to have such a huge absorptive surface area packed into a relatively small space:
- Mucosal folds: The inner surface of the small intestine is not flat, but thrown into circular folds. This not only increases the surface area, but helps regulate the flow of digested food through your intestine.
- Villi: The folds form numerous tiny projections which stick out into the open space inside your small intestine (or lumen), and are covered with cells that help absorb nutrients from the food that passes through.
- Microvilli: The cells on the villi are packed full of tiny hair like structures called microvilli. This helps increase the surface of each individual cell, meaning that each cell can absorb more nutrients.
THE COLON
Finally, any nutrient that is not broken small enough to cross the small intestinal wall will be transported into the large intestine (colon). And so it is important to emphasize that effective chewing plays a role in initially grinding food before swallowing. Just imagine eating the leafy greens in your salad and then excreting them almost unchanged! The leaves could have been digested effectively when it is chewed properly. In a healthy person, only approximately five percent of a meal reaches the colon and can remain in the large intestine for about 24-72 hours, depending on the fiber and fluid content of the meal. The large intestine contains water, sodium, potassium, small amounts of undigested starches, and microflora, which are bacteria that help, keep the colon healthy. Colon bacteria are also responsible for producing gas as a by-product of their digestion of fiber or other waste. Diets adequate in fluid and fiber generally result in stools that are soft and easily passed through the rectum. Diets inadequate in fluid and fiber may result in hard, dry stools. These digestive waste products should be eliminated regularly; we don’t want to keep them.
Finally, any nutrient that is not broken small enough to cross the small intestinal wall will be transported into the large intestine (colon). And so it is important to emphasize that effective chewing plays a role in initially grinding food before swallowing. Just imagine eating the leafy greens in your salad and then excreting them almost unchanged! The leaves could have been digested effectively when it is chewed properly. In a healthy person, only approximately five percent of a meal reaches the colon and can remain in the large intestine for about 24-72 hours, depending on the fiber and fluid content of the meal. The large intestine contains water, sodium, potassium, small amounts of undigested starches, and microflora, which are bacteria that help, keep the colon healthy. Colon bacteria are also responsible for producing gas as a by-product of their digestion of fiber or other waste. Diets adequate in fluid and fiber generally result in stools that are soft and easily passed through the rectum. Diets inadequate in fluid and fiber may result in hard, dry stools. These digestive waste products should be eliminated regularly; we don’t want to keep them.
Absorption of water into the bloodstream slowly reduces the water content of the material left inside the large intestine, and the water product has a solid consistency. This solid material is the feces. Mucus, the only secretion of the large intestine, provides lubrication for the smooth passage of the feces. By the time feces reach the rectum, it consists of 75 percent water and 25 percent solids. The solids include cellular wastes, undigested dietary fiber, undigested food, bile salts, cholesterol, mucus, and bacteria. The body cannot digest some forms of carbohydrates because it lacks the necessary enzyme to split the appropriate molecule. Some vegetables and legumes contain these indigestible sugars and fibers. Intestinal gas is formed in the colon by the decomposition of undigested materials. Examples of gas-forming foods are beans, onions, radishes, and vegetables of the cabbage family.
THE ACCESSORY ORGANS
Apart from the alimentary canal, three accessory organs are considered part of the digestive system located outside of the alimentary canal - the liver, gallbladder, and pancreas. They all play essential roles in the digestive process. The pancreas, apart from producing insulin (endocrine function) secretes enzymes collectively known as pancreatic juice that are involved in the digestion of all the energy nutrients. Pancreatic juice is carried to the small intestine through the pancreatic and common bile duct. The liver is the second largest organ in the body that performs many functions primarily the production of bile which is important in breaking down dietary fats.
The gallbladder is a 3-to-4-inch sac that concentrates and stores bile until it is needed in the small intestine. Bile is delivered to the small intestine through the common bile duct (where gallstones are usually trapped causing obstruction). About 2 to 3 cups of bile are secreted each day into the alimentary canal. There is a growing global burden of Gallstone disease according to the World Gastroenterology Organization.
Many chemical reactions are involved in digestion with more than 500 enzymes needed in the process. In addition to enzymes, other secretions and chemicals are used including mucus, electrolytes, and water. The control of secretions, chemicals and enzymes during the digestive process is influenced by several factors. Emotions and conditioned responses can affect the amount of a secretion released. The smell of food, for example, will cause the release of hydrochloric acid in the stomach.
Nervousness or stress can affect digestion time where it can either speeds up or slows down digestion. For example, if an individual is stressed and has consumed food, it may stay longer than normal and produce an uncomfortable heavy feeling. But on the other hand, another person with the same level of stress might experience rapid digestion and may result to diarrhea.
Apart from the alimentary canal, three accessory organs are considered part of the digestive system located outside of the alimentary canal - the liver, gallbladder, and pancreas. They all play essential roles in the digestive process. The pancreas, apart from producing insulin (endocrine function) secretes enzymes collectively known as pancreatic juice that are involved in the digestion of all the energy nutrients. Pancreatic juice is carried to the small intestine through the pancreatic and common bile duct. The liver is the second largest organ in the body that performs many functions primarily the production of bile which is important in breaking down dietary fats.
The gallbladder is a 3-to-4-inch sac that concentrates and stores bile until it is needed in the small intestine. Bile is delivered to the small intestine through the common bile duct (where gallstones are usually trapped causing obstruction). About 2 to 3 cups of bile are secreted each day into the alimentary canal. There is a growing global burden of Gallstone disease according to the World Gastroenterology Organization.
Many chemical reactions are involved in digestion with more than 500 enzymes needed in the process. In addition to enzymes, other secretions and chemicals are used including mucus, electrolytes, and water. The control of secretions, chemicals and enzymes during the digestive process is influenced by several factors. Emotions and conditioned responses can affect the amount of a secretion released. The smell of food, for example, will cause the release of hydrochloric acid in the stomach.
Nervousness or stress can affect digestion time where it can either speeds up or slows down digestion. For example, if an individual is stressed and has consumed food, it may stay longer than normal and produce an uncomfortable heavy feeling. But on the other hand, another person with the same level of stress might experience rapid digestion and may result to diarrhea.