UNIT 2 - LIVER AND GALLBLADDER DISEASE MANAGEMENT |
OBJECTIVES:
- identify the risk factors for Alcoholic & Toxic Liver
- Understand the nutritional consideration for Cirrhosis of the liver
- Nutrition Guide for Clinicians, Neal Barnard, MD, 2009
- Nutrition Facts, Michel Greger, MD
Alcoholic and Toxic Liver
The liver is responsible for concentrating and metabolizing most drugs and toxins. Because of this function, toxic insults to the liver are common. In the US, drug-induced liver injury (DILI) is the most common cause of acute liver failure. Alcohol-related liver disease accounts for more than 12,000 deaths yearly in the United States, and alcohol abuse is the most common cause of cirrhosis.
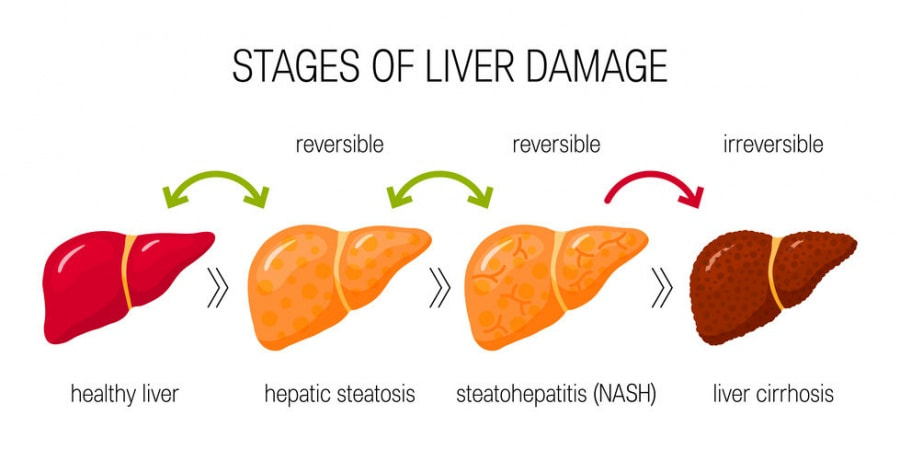
Alcohol is the most frequently abused drug worldwide. Its major metabolite, acetaldehyde, is directly toxic to the liver. Abuse results in a broad spectrum of liver disease, including asymptomatic fatty liver, alcoholic hepatitis, cirrhosis, and end-stage liver failure. Many alcoholics become symptomatic only when severe, life-threatening liver disease is already present. Virtually any drug can cause some degree of hepatotoxicity, although certain drugs are more toxic than others. In some cases (e.g., sulfonamides), substances are directly toxic to the liver.
In others, liver damage occurs by immune-mediated hypersensitivity. Some common hepatotoxic substances include acetaminophen, antibiotics (most commonly amoxicillin-clavulanate), tetracycline, aspirin, phenytoin, methyldopa, isoniazid, methotrexate (when combined with alcohol), HMG-CoA reductase inhibitors (“statins”), and valproic acid. In high doses, vitamin A, arsenic, iron, and copper can be hepatotoxic. Hepatotoxicity from use of herbal and dietary supplements accounts for about 20% of all cases of drug-induced liver injury,[3] and may be the most common serious adverse effect of herbal supplements. Known hepatotoxic herbs include Ayurvedic herbs, kava, pennyroyal oil, Ma-huang ( Ephedra sinica), valerian, mistletoe, comfrey, chaparral, sassafras, borage, and germander.
The presentation and severity of liver disease vary widely. Some patients remain asymptomatic despite significant liver damage, while others present with a severe, acute illness. Nausea, vomiting, malaise, and diaphoresis are common symptoms. A syndrome similar to viral hepatitis may occur, including fever, headache, jaundice, and right-upper-quadrant pain. Pruritus may occur if cholestasis develops. Jaundice is a common presentation in people with alcoholic hepatitis. Hepatic encephalopathy and coagulopathies may develop in severe instances. Because of the liver’s regenerative ability, withdrawal of or abstinence from offending substances can sometimes result in significant reversal of liver damage, even in cases of advanced liver disease, so long as cirrhosis is not yet established.
RISK FACTORS
Alcohol use. Sustained alcohol intake exceeding 30 g per day (one standard alcoholic drink has 14 g) is associated with progression to cirrhosis and non-cirrhotic liver damage in both men and women. Binge drinking, drinking alcohol outside of meal times, and drinking beer or hard alcohol versus wine have all been associated with increased rates of liver damage.
Sex. Females have an increased risk of liver disease for a given amount and duration of alcohol use, and liver disease in women tends to progress more rapidly than in men.
Genetics. There appear to be genetic predispositions to alcohol abuse and alcoholic liver disease. However, specific genes have yet to be definitely identified.
Viral hepatitis. Concurrent infection with hepatitis B virus or hepatitis C virus is strongly associated with risk of accelerated liver disease in alcoholic patients.
Obesity/Malnutrition. Inadequate nutritional intake in chronic alcohol abusers may worsen the severity of liver disease.
Race. Many Asians have a relative deficiency of the mitochondrial aldehyde dehydrogenase-2 (ALDH2) enzyme, which results in flushing upon alcohol intake and may create an aversion to alcohol use in these populations. Hispanic and African-American males tend to have higher rates of cirrhosis in comparison to Caucasian men, irrespective of the quantity of alcohol ingested.
Acetaminophen. The combination of alcohol and acetaminophen should be avoided, as acetaminophen toxicity is greatly increased with the concomitant ingestion of alcohol.
Drug dosages. Toxicity due to medications is typically dose-related.
Nutritional supplements. High doses of preformed vitamin A can be hepatotoxic, as can certain botanicals.
Alcohol is the most frequently abused drug worldwide. Its major metabolite, acetaldehyde, is directly toxic to the liver. Abuse results in a broad spectrum of liver disease, including asymptomatic fatty liver, alcoholic hepatitis, cirrhosis, and end-stage liver failure. Many alcoholics become symptomatic only when severe, life-threatening liver disease is already present. Virtually any drug can cause some degree of hepatotoxicity, although certain drugs are more toxic than others. In some cases (e.g., sulfonamides), substances are directly toxic to the liver.
In others, liver damage occurs by immune-mediated hypersensitivity. Some common hepatotoxic substances include acetaminophen, antibiotics (most commonly amoxicillin-clavulanate), tetracycline, aspirin, phenytoin, methyldopa, isoniazid, methotrexate (when combined with alcohol), HMG-CoA reductase inhibitors (“statins”), and valproic acid. In high doses, vitamin A, arsenic, iron, and copper can be hepatotoxic. Hepatotoxicity from use of herbal and dietary supplements accounts for about 20% of all cases of drug-induced liver injury,[3] and may be the most common serious adverse effect of herbal supplements. Known hepatotoxic herbs include Ayurvedic herbs, kava, pennyroyal oil, Ma-huang ( Ephedra sinica), valerian, mistletoe, comfrey, chaparral, sassafras, borage, and germander.
The presentation and severity of liver disease vary widely. Some patients remain asymptomatic despite significant liver damage, while others present with a severe, acute illness. Nausea, vomiting, malaise, and diaphoresis are common symptoms. A syndrome similar to viral hepatitis may occur, including fever, headache, jaundice, and right-upper-quadrant pain. Pruritus may occur if cholestasis develops. Jaundice is a common presentation in people with alcoholic hepatitis. Hepatic encephalopathy and coagulopathies may develop in severe instances. Because of the liver’s regenerative ability, withdrawal of or abstinence from offending substances can sometimes result in significant reversal of liver damage, even in cases of advanced liver disease, so long as cirrhosis is not yet established.
RISK FACTORS
Alcohol use. Sustained alcohol intake exceeding 30 g per day (one standard alcoholic drink has 14 g) is associated with progression to cirrhosis and non-cirrhotic liver damage in both men and women. Binge drinking, drinking alcohol outside of meal times, and drinking beer or hard alcohol versus wine have all been associated with increased rates of liver damage.
Sex. Females have an increased risk of liver disease for a given amount and duration of alcohol use, and liver disease in women tends to progress more rapidly than in men.
Genetics. There appear to be genetic predispositions to alcohol abuse and alcoholic liver disease. However, specific genes have yet to be definitely identified.
Viral hepatitis. Concurrent infection with hepatitis B virus or hepatitis C virus is strongly associated with risk of accelerated liver disease in alcoholic patients.
Obesity/Malnutrition. Inadequate nutritional intake in chronic alcohol abusers may worsen the severity of liver disease.
Race. Many Asians have a relative deficiency of the mitochondrial aldehyde dehydrogenase-2 (ALDH2) enzyme, which results in flushing upon alcohol intake and may create an aversion to alcohol use in these populations. Hispanic and African-American males tend to have higher rates of cirrhosis in comparison to Caucasian men, irrespective of the quantity of alcohol ingested.
Acetaminophen. The combination of alcohol and acetaminophen should be avoided, as acetaminophen toxicity is greatly increased with the concomitant ingestion of alcohol.
Drug dosages. Toxicity due to medications is typically dose-related.
Nutritional supplements. High doses of preformed vitamin A can be hepatotoxic, as can certain botanicals.
Cirrhosis of the liver
Cirrhosis is a condition of diffuse hepatic fibrosis with replacement of the normal liver architecture by nodules. It is the final pathway for a wide variety of chronic liver diseases.Progression of chronic liver disease to cirrhosis can take anywhere from weeks to years, depending on the disease etiology. Cirrhosis is a leading cause of mortality during the most productive years of life. There is no treatment to reverse cirrhosis.A wide variety of chronic liver diseases lead to cirrhosis. The most common are toxic/metabolic (alcohol, non-alcoholic fatty liver disease, hemochromatosis), viral (hepatitis B and C) and autoimmune (autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis). Less common etiologies include biliary (atresia, stone, tumor), vascular (Budd-Chiari, cardiac), genetic (cystic fibrosis, lysosomal acid lipase deficiency), metabolic (alpha-1-antitrypsin deficiency, galactosemia, Wilson’s disease) and iatrogenic (biliary injury, drugs) conditions.Cirrhosis can be classified as compensated or decompensated. Patients with compensated cirrhosis are often asymptomatic and may have no abnormalities on physical examination, laboratory tests, or imaging. Cirrhosis is called decompensated in the presence of hepatic encephalopathy, variceal bleeding, ascites, or jaundice.
Varices is not uncommon and can result in massive hematemesis and high mortality. Patients with decompensated disease may also develop complications involving other organ systems, including renal failure due to hepatorenal syndrome, hypoxia caused by hepatopulmonary syndrome, pulmonary hypertension secondary to portopulmonary hypertension, or heart failure secondary to cirrhotic cardiomyopathy. The risk of liver cancer in patients with cirrhosis is estimated at about 1%-2% per year. Treatment of the underlying etiology of disease can occasionally revert decompensated cirrhosis back to a compensated state. However, those who do not improve with treatment should be considered for liver transplantation.
RISK FACTORS
Alcohol related disease. Alcohol-use disorder is one of the main causes of liver disease and associated mortality. Approximately 1 in 12 adults have alcohol-use disorder defined as consumption of > 3 drinks per day in men and > 2 drinks in women, or binge drinking (defined as > 5 drinks in males and > 4 drinks in females, consumed over a 2-hour period). One drink is defined as a beverage containing 14 g of alcohol, which is approximately 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of hard liquor.
Viral hepatitis. Established risk factors for the acquisition of chronic hepatitis B (HBV) and C (HCV) include intravenous drug use, chronic hemodialysis, blood transfusion or transplantation prior to 1992 (HCV), receipt of blood (including needle stick) from a person with HCV, receipt of clotting factor concentrates products before 1987, Asian ancestry (HBV), lack of vaccination (for healthcare workers) (HBV), and childbirth from a mother with chronic HBV or HCV. Possible risk factors include body piercing or tattoos, multiple sexual partners, sexually transmitted diseases, work in healthcare (HCV), and contacts with HCV-positive persons.
Non-alcoholic fatty liver disease (NAFLD). Risk factors for the development of NAFLD include features of the metabolic syndrome, including type 2 diabetes, hyperlipidemia, hypertriglyceridemia, obesity (body mass index > 30 kg/m2), increased waist circumference (> 89 cm in women and > 102 cm in men) and reduced high-density lipoprotein (HDL) cholesterol (< 40 mg/dL in men and < 50 mg/dL in women). Other conditions associated with NAFLD include polycystic ovarian syndrome, obstructive sleep apnea, hypothyroidism, and hypopituitarism.
Medications. Long-term use of methotrexate, amiodarone, and tamoxifen can cause hepatic fibrosis and cirrhosis in certain patients.
Alcohol related disease. Alcohol-use disorder is one of the main causes of liver disease and associated mortality. Approximately 1 in 12 adults have alcohol-use disorder defined as consumption of > 3 drinks per day in men and > 2 drinks in women, or binge drinking (defined as > 5 drinks in males and > 4 drinks in females, consumed over a 2-hour period). One drink is defined as a beverage containing 14 g of alcohol, which is approximately 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of hard liquor.
Viral hepatitis. Established risk factors for the acquisition of chronic hepatitis B (HBV) and C (HCV) include intravenous drug use, chronic hemodialysis, blood transfusion or transplantation prior to 1992 (HCV), receipt of blood (including needle stick) from a person with HCV, receipt of clotting factor concentrates products before 1987, Asian ancestry (HBV), lack of vaccination (for healthcare workers) (HBV), and childbirth from a mother with chronic HBV or HCV. Possible risk factors include body piercing or tattoos, multiple sexual partners, sexually transmitted diseases, work in healthcare (HCV), and contacts with HCV-positive persons.
Non-alcoholic fatty liver disease (NAFLD). Risk factors for the development of NAFLD include features of the metabolic syndrome, including type 2 diabetes, hyperlipidemia, hypertriglyceridemia, obesity (body mass index > 30 kg/m2), increased waist circumference (> 89 cm in women and > 102 cm in men) and reduced high-density lipoprotein (HDL) cholesterol (< 40 mg/dL in men and < 50 mg/dL in women). Other conditions associated with NAFLD include polycystic ovarian syndrome, obstructive sleep apnea, hypothyroidism, and hypopituitarism.
Medications. Long-term use of methotrexate, amiodarone, and tamoxifen can cause hepatic fibrosis and cirrhosis in certain patients.
Article Review
Video Review
|
|
|
Unit Task
Submit your Reflective Journal after watching the videos, reading the lesson and article.