UNIT 3 - LIVER AND GALLBLADDER DISEASE MANAGEMENT |
OBJECTIVES:
- Describe gallstone disease.
- Identify the risk factors for gallstone disease.
- Understand the nutritional consideration for gallstone disease.
- Neal Barnard, MD, (2009). Nutrition Guide for Clinicians.
- Michael Greger, MD, (2011). Nutrition Facts.
- John McDougal, MD, (2011). McDougal Health & Medical Center.
- Klaper, M., (2019). Dr. Klaper Channel.
Gallstone Disease
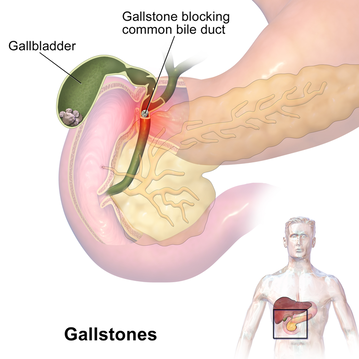
Gallstone disease is a condition in which hard stones composed of cholesterol or bile pigments form in the gallbladder (cholecystolithiasis) or common bile duct (choledocholithiasis). In the US about 9% of women and 6% of men have gallstones and most are asymptomatic.
Most stones are composed of cholesterol. In bile, cholesterol is in equilibrium with bile salts and phosphatidylcholine. When the concentration of cholesterol rises to the point of supersaturation, crystallization occurs. A sludge containing cholesterol, mucin, calcium salts, and bilirubin forms, and, ultimately, stones develop. Although gallstones are typically asymptomatic, some cause biliary colic, in which stones intermittently obstruct the neck of the gallbladder and/or the common bile duct and cause episodic right-upper-quadrant abdominal pain.
Chronic obstruction may result in cholecystitis (infection and inflammation of the gallbladder) or cholangitis (infection and inflammation of the common bile duct). Both syndromes are serious and, if untreated, may result in sepsis, shock, and death. Presenting symptoms include episodic right-upper-quadrant or epigastric pain, which often occurs in the middle of the night after eating a large meal and may radiate to the back, right scapula, or right shoulder. Diaphoresis, nausea, vomiting, dyspepsia, burping, and food intolerance (especially to fatty, greasy, or fried foods; meats; and cheeses) are common. More severe symptoms, including fever and jaundice, may signify cholecystitis or cholangitis.
Most stones are composed of cholesterol. In bile, cholesterol is in equilibrium with bile salts and phosphatidylcholine. When the concentration of cholesterol rises to the point of supersaturation, crystallization occurs. A sludge containing cholesterol, mucin, calcium salts, and bilirubin forms, and, ultimately, stones develop. Although gallstones are typically asymptomatic, some cause biliary colic, in which stones intermittently obstruct the neck of the gallbladder and/or the common bile duct and cause episodic right-upper-quadrant abdominal pain.
Chronic obstruction may result in cholecystitis (infection and inflammation of the gallbladder) or cholangitis (infection and inflammation of the common bile duct). Both syndromes are serious and, if untreated, may result in sepsis, shock, and death. Presenting symptoms include episodic right-upper-quadrant or epigastric pain, which often occurs in the middle of the night after eating a large meal and may radiate to the back, right scapula, or right shoulder. Diaphoresis, nausea, vomiting, dyspepsia, burping, and food intolerance (especially to fatty, greasy, or fried foods; meats; and cheeses) are common. More severe symptoms, including fever and jaundice, may signify cholecystitis or cholangitis.
RISK FACTORS
Family history. Gallstones are more than twice as common in first-degree relatives of individuals with gallstones.
Increasing age. Gallstones are most common in individuals over age 40.
Female sex. Females are more likely to develop gallstones in all age groups, probably due to the effects of estrogens. This increased risk is most notable in young women, who are affected 3-4 times more often than men of the same age.
Elevated estrogen and progesterone. During pregnancy, oral contraceptive use, or hormone replacement therapy, estrogen and progesterone induce changes in the biliary system that predispose to gallstones.
Obesity. Obesity is a significant risk factor for the development of cholesterol gallstones due to elevated production and secretion of cholesterol.
Rapid weight loss. Bariatric surgery and very-low-calorie diets increase risk of gallstone formation, possibly due to increased concentrations of bile constituents.
Diabetes mellitus. High triglycerides, gallbladder stasis, and hepatic insulin resistance may increase risk of gallstones.[1]Gallbladder stasis. When bile remains in the gallbladder for an extended period, supersaturation can occur. Gallbladder stasis is associated with diabetes mellitus, total parenteral nutrition (probably due to lack of enteral stimulation), vagotomy, rapid weight loss, celiac sprue, and spinal cord injury.
Cirrhosis. Cirrhosis leads to as much as a 10-fold increased risk of gallstones.
Ileal disease or resection (as in Crohn’s disease). Changes in enterohepatic cycling of bile salts increases risk of gallstone formation.
Hemolytic states. The rapid destruction of red blood cells in sickle cell disease and other hemolytic conditions causes the release of bilirubin, which in turn increases the risk of pigment gallstones.
Medications. Drugs implicated in the development of cholelithiasis include clofibrate, octreotide, and ceftriaxone.
Physical inactivity. Exercise may reduce gallstone risk. Findings from the Health Professionals Follow-up Study suggested that the risk of symptomatic cholelithiasis could be reduced by 30 minutes of daily aerobic exercise. Young or middle-aged men (65 years or younger) who were the most physically active had half the risk for developing gallstones, compared with those who were least active. In older men, physical activity cut risk by 25%. Physical activity is also associated with reduced gallstone risk in women.
Family history. Gallstones are more than twice as common in first-degree relatives of individuals with gallstones.
Increasing age. Gallstones are most common in individuals over age 40.
Female sex. Females are more likely to develop gallstones in all age groups, probably due to the effects of estrogens. This increased risk is most notable in young women, who are affected 3-4 times more often than men of the same age.
Elevated estrogen and progesterone. During pregnancy, oral contraceptive use, or hormone replacement therapy, estrogen and progesterone induce changes in the biliary system that predispose to gallstones.
Obesity. Obesity is a significant risk factor for the development of cholesterol gallstones due to elevated production and secretion of cholesterol.
Rapid weight loss. Bariatric surgery and very-low-calorie diets increase risk of gallstone formation, possibly due to increased concentrations of bile constituents.
Diabetes mellitus. High triglycerides, gallbladder stasis, and hepatic insulin resistance may increase risk of gallstones.[1]Gallbladder stasis. When bile remains in the gallbladder for an extended period, supersaturation can occur. Gallbladder stasis is associated with diabetes mellitus, total parenteral nutrition (probably due to lack of enteral stimulation), vagotomy, rapid weight loss, celiac sprue, and spinal cord injury.
Cirrhosis. Cirrhosis leads to as much as a 10-fold increased risk of gallstones.
Ileal disease or resection (as in Crohn’s disease). Changes in enterohepatic cycling of bile salts increases risk of gallstone formation.
Hemolytic states. The rapid destruction of red blood cells in sickle cell disease and other hemolytic conditions causes the release of bilirubin, which in turn increases the risk of pigment gallstones.
Medications. Drugs implicated in the development of cholelithiasis include clofibrate, octreotide, and ceftriaxone.
Physical inactivity. Exercise may reduce gallstone risk. Findings from the Health Professionals Follow-up Study suggested that the risk of symptomatic cholelithiasis could be reduced by 30 minutes of daily aerobic exercise. Young or middle-aged men (65 years or younger) who were the most physically active had half the risk for developing gallstones, compared with those who were least active. In older men, physical activity cut risk by 25%. Physical activity is also associated with reduced gallstone risk in women.
Nutritional Consideration
Gallstones are strongly related to high-fat, low-fiber diets. They are uncommon in Asian and African populations that follow traditional, largely plant-based diets, and they become more common with a shift toward Westernized diets.[6] A surplus of animal protein and animal fat, a lack of dietary fiber, and the consumption of fat from saturated rather than unsaturated sources appear to be the main nutritional risk factors for gallstone development.
The following factors are associated with reduced risk of gallstones:
Plant-based diets. Both animal fat and animal protein may contribute to the formation of gallstones. Up to 90% of gallstones are cholesterol stones (≥ 20% cholesterol composition), suggesting the possibility that dietary changes (e.g., reducing dietary saturated fat and cholesterol and increasing soluble fiber) may reduce the risk of gallstones. Vegetarian women have a lower risk for gallstones, compared with nonvegetarian women. Vegetarian diets are often high in fiber and provide fat mainly in its unsaturated forms. Fruit and vegetable intake may account for part of this protection. Consuming abundant amounts fruits and vegetables is associated with reduced risk for cholecystectomy.
Vitamin C, which is found in plants and is absent from meat, affects the rate-limiting step in the catabolism of cholesterol to bile acids and is inversely related to the risk of gallstones in women. Women consuming the most vegetable protein have been shown to have a 20-30% lower risk than those consuming the least. Similarly, women and men whose fat intake comes primarily from plant sources have a reduced risk of developing gallstones. An exception is trans fatty acids—the partially hydrogenated vegetable oils often used in snack foods—which are associated with increased gallstone risk.
Within the general population, high LDL cholesterol levels are associated with gallstone formation, emphasizing the importance of a diet (i.e., high-fiber, low-fat) that keeps blood lipids in a healthy range. Replacement of sugars and refined starches with high-fiber foods. The cholesterol saturation index of bile, a known risk factor for gallstone formation, is higher with diets that provide carbohydrates in a refined, as opposed to unrefined, form. In a 12 year prospective cohort study among U.S. men, individuals consuming the most refined carbohydrates have a 60% greater risk for developing gallstones, compared with those who consumed the least.
Conversely, in a 1998 cross-sectional study of men and women in Italy, individuals eating the most fiber (particularly insoluble fiber) have a 15% lower risk for gallstones compared with those eating the least. Avoidance of excess weight and a healthful approach to weight control. Women with a BMI of ≥30 kg/m2 have at least double the risk for gallstone disease, compared with women with a BMI < 25 kg/m2). The same degree of risk exists for men with a BMI of at least 25 kg/m2, compared with a BMI of < 22.5 kg/m2. Risk rises with increasing obesity.[21]Weight cycling (repeatedly intentionally losing and unintentionally regaining weight) increases the likelihood of cholelithiasis. In a 1999 prospective cohort study of 47,153 women in 11 U.S. states, the risk for cholecystectomy increased from 20% in “light” cyclers (those who lost and regained five to nine pounds) to 70% in “severe” cyclers (those who lost and regained ≥ 20 pounds).
A 2006 study of U.S. men shows a similar pattern. As noted above, very-low-calorie diets (< 800 kcal/day) increase the risk of gallstones, though the explanation for this remains unclear. Including a small amount of fat (10 g/day) provides maximal gallbladder emptying and prevents gallstone formation in calorie-restricted dieters. Such observations support weight control efforts based on low-fat, plant-based diets, which typically cause healthful and sustained weight control, rather than those based on very-low-calorie formula diets.
Moderate alcohol intake. Compared with infrequent consumption or abstinence, moderate alcohol intake was found to be inversely associated with the risk for gallstones. However, given the health risks (e.g., breast or colorectal cancer) associated with alcohol consumption, caution regarding alcohol use is warranted.
The following factors are associated with reduced risk of gallstones:
Plant-based diets. Both animal fat and animal protein may contribute to the formation of gallstones. Up to 90% of gallstones are cholesterol stones (≥ 20% cholesterol composition), suggesting the possibility that dietary changes (e.g., reducing dietary saturated fat and cholesterol and increasing soluble fiber) may reduce the risk of gallstones. Vegetarian women have a lower risk for gallstones, compared with nonvegetarian women. Vegetarian diets are often high in fiber and provide fat mainly in its unsaturated forms. Fruit and vegetable intake may account for part of this protection. Consuming abundant amounts fruits and vegetables is associated with reduced risk for cholecystectomy.
Vitamin C, which is found in plants and is absent from meat, affects the rate-limiting step in the catabolism of cholesterol to bile acids and is inversely related to the risk of gallstones in women. Women consuming the most vegetable protein have been shown to have a 20-30% lower risk than those consuming the least. Similarly, women and men whose fat intake comes primarily from plant sources have a reduced risk of developing gallstones. An exception is trans fatty acids—the partially hydrogenated vegetable oils often used in snack foods—which are associated with increased gallstone risk.
Within the general population, high LDL cholesterol levels are associated with gallstone formation, emphasizing the importance of a diet (i.e., high-fiber, low-fat) that keeps blood lipids in a healthy range. Replacement of sugars and refined starches with high-fiber foods. The cholesterol saturation index of bile, a known risk factor for gallstone formation, is higher with diets that provide carbohydrates in a refined, as opposed to unrefined, form. In a 12 year prospective cohort study among U.S. men, individuals consuming the most refined carbohydrates have a 60% greater risk for developing gallstones, compared with those who consumed the least.
Conversely, in a 1998 cross-sectional study of men and women in Italy, individuals eating the most fiber (particularly insoluble fiber) have a 15% lower risk for gallstones compared with those eating the least. Avoidance of excess weight and a healthful approach to weight control. Women with a BMI of ≥30 kg/m2 have at least double the risk for gallstone disease, compared with women with a BMI < 25 kg/m2). The same degree of risk exists for men with a BMI of at least 25 kg/m2, compared with a BMI of < 22.5 kg/m2. Risk rises with increasing obesity.[21]Weight cycling (repeatedly intentionally losing and unintentionally regaining weight) increases the likelihood of cholelithiasis. In a 1999 prospective cohort study of 47,153 women in 11 U.S. states, the risk for cholecystectomy increased from 20% in “light” cyclers (those who lost and regained five to nine pounds) to 70% in “severe” cyclers (those who lost and regained ≥ 20 pounds).
A 2006 study of U.S. men shows a similar pattern. As noted above, very-low-calorie diets (< 800 kcal/day) increase the risk of gallstones, though the explanation for this remains unclear. Including a small amount of fat (10 g/day) provides maximal gallbladder emptying and prevents gallstone formation in calorie-restricted dieters. Such observations support weight control efforts based on low-fat, plant-based diets, which typically cause healthful and sustained weight control, rather than those based on very-low-calorie formula diets.
Moderate alcohol intake. Compared with infrequent consumption or abstinence, moderate alcohol intake was found to be inversely associated with the risk for gallstones. However, given the health risks (e.g., breast or colorectal cancer) associated with alcohol consumption, caution regarding alcohol use is warranted.
Article Review
Plant-Based Diet, Cholesterol, and Risk of Gallstone Disease: A Prospective Study
Association between diet and gallstones of cholesterol and pigment among patients with cholecystectomy: a case-control study in Korea
Association between diet and gallstones of cholesterol and pigment among patients with cholecystectomy: a case-control study in Korea
Video Review
|
|
|
|
|
|
Unit Task
Submit your Reflective Journal after watching the videos, reading the lesson and article.