Cancer Prevention & Management
UNIT 2 |
OBJECTIVES
SOURCES
- Explore the unique metabolism of Cancer cell
- Discuss the lifestyle related cause of the following:
- Breast Cancer
- Prostate Cancer
- Gastrointestinal Cancer
- Blood Cancer
- Breast Cancer
SOURCES
- Undo It, Dean Ornish, MD
- How not to Die, Michael Greger, MD
- Nutrition Guide for Nutrition 2nd Edition, Neal Barnard, MD
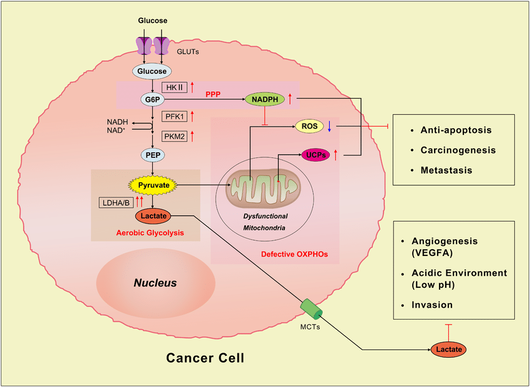
Cancer Cell Metabolism
A normal body also has additional reserves to suppress and destroy malignancies. It does not act in that manner in cancer patients, where the cancer grew from the smallest cellular unit freely, without encountering any resistance. What forces can suppress such a development? This can be accomplished by the oxidizing enzyme and the conditions which maintain their activity. The best known oxidizing enzymes are:
All these are lower in activity in both fetal liver and hepatoma than in normal or regenerating liver. Otto Warburg was the first who found the metabolic deviations of malignant tissue from normal tissue and formulated it by the co-efficient: anaerobic glycolysis / cell respiration.
In normal tissue it is zero
In embryonic tissue 0.1
In benign tumors 0.45 to 1.45
In malignant tissue up to 12.
It is known that in primitive forms of life the energy of the cells is derived almost entirely from anaerobic conditions or through fermentation. In higher form of animals, the lower fermentative anerobic systems are mixed with oxidation systems, whereby more and more molecular oxygen is utilized, transported from the respiration of the lungs. The malignancies in human beings continuously fall back deeper into fermentation.
In the nutritional fields, observations for centuries have shown that people who live according to natural methods in which plants, animals and human beings are only fragments of the eternal cycle of Nature do not get cancer. On the contrary, people who accept methods of modern nutrition on an increasing scale become involved in degenerative diseases, including cancer, in a relatively short time.
The best known cancer-free people were the Hunzas, who live on the slopes of the Himalaya mountains and who use only food grown in their own country and fertilized with natural manure. Imported food is forbidden. Very similar is the story of the Ethiopians who also have natural agriculture and living habits which seems to prove that this type of agriculture keeps people free of cancer and most of the degenerative diseases.
DIET DURING CANCER TREATMENT
There are no standard evidence-based recommendations for diet therapy during cancer treatment, due in part to the heterogeneous nature of this disease. Loss of appetite an severe weight loss (cachexia) are common in many cancer patients, and significant weight loss at the time of diagnosis - as well as malnutrition that may occur during the course of the disease - is a predictor of poor outcome. Malnutrition also impairs the response to chemotherapy. Due to these risks, the National Cancer Institute (NCI) suggests early nutrition screening and intervention, as well as close monitoring and evaluation of patients throughout all phases of cancer treatment and recovery.
NUTRITION ASSESSMENT GOALS, CRITERIA, and METHODOLOGY
The goals of nutrition assessment and therapy include prevention or reversal of nutrient deficiencies; preservation of lean body mass; increased tolerance for anticancer treatments with a minimization of nutrition-related side effects and complications; decreased risk for infection through support of immune function; facilitation of recovery and healing; and maintenance of strength, energy, and quality of life.
POTENTIAL RISK OF AGGRESSIVE NUTRITION THERAPY
Because weight loss and malnutrition are often significant in individuals fighting malignancy, clinical efforts frequency focus on increasing protein and energy intake by any means acceptable to patients, including use of the same type of cuisine that might have contributed to the initial development of the malignancy and that may be associated with poorer long-term survival. Although identification of nutrition problems and treatment of nutrition-related symptoms have been shown to stabilize or reverse weight loss in 50% to 88% of oncology patients, there is little evidence that these patients survive longer than patients whose weight loss is less aggressively treated. Evidence suggests that ad libitum diets high in fat, sugar, and animal protein may, by increasing cancer growth factors and stimulating cellular events leading to immune suppression and inflammation, foster cell proliferation and metastasis, interfere with effective treatment, and potentially worsen survival. These issues await further research.
Weight loss may lead to cachexia should be differentiated from healthful weight loss in overweight individuals. In certain cancers (eg, breast and colon), higher weight and/or greater percent body fat have been associated with increased mortality after diagnosis. One study of 526 individuals with colon cancer found that every 10% increase in body fat was associated with a 33% decrease in cancer survival. Caution should therefore be exercised in trying to prevent weight loss in individuals for whom such loss would otherwise be therapeutic, particularly in light of findings that adipocytes secrete adipocytokines (eg, leptin) that have an agonistic effect on cancer growth.
GASTROINTESTINAL DISTURBANCES
The National Cancer Institute and the American Cancer Society suggest the following dietary strategies to control the nausea and vomiting associated with chemotherapy.
In normal tissue it is zero
In embryonic tissue 0.1
In benign tumors 0.45 to 1.45
In malignant tissue up to 12.
It is known that in primitive forms of life the energy of the cells is derived almost entirely from anaerobic conditions or through fermentation. In higher form of animals, the lower fermentative anerobic systems are mixed with oxidation systems, whereby more and more molecular oxygen is utilized, transported from the respiration of the lungs. The malignancies in human beings continuously fall back deeper into fermentation.
In the nutritional fields, observations for centuries have shown that people who live according to natural methods in which plants, animals and human beings are only fragments of the eternal cycle of Nature do not get cancer. On the contrary, people who accept methods of modern nutrition on an increasing scale become involved in degenerative diseases, including cancer, in a relatively short time.
The best known cancer-free people were the Hunzas, who live on the slopes of the Himalaya mountains and who use only food grown in their own country and fertilized with natural manure. Imported food is forbidden. Very similar is the story of the Ethiopians who also have natural agriculture and living habits which seems to prove that this type of agriculture keeps people free of cancer and most of the degenerative diseases.
DIET DURING CANCER TREATMENT
There are no standard evidence-based recommendations for diet therapy during cancer treatment, due in part to the heterogeneous nature of this disease. Loss of appetite an severe weight loss (cachexia) are common in many cancer patients, and significant weight loss at the time of diagnosis - as well as malnutrition that may occur during the course of the disease - is a predictor of poor outcome. Malnutrition also impairs the response to chemotherapy. Due to these risks, the National Cancer Institute (NCI) suggests early nutrition screening and intervention, as well as close monitoring and evaluation of patients throughout all phases of cancer treatment and recovery.
NUTRITION ASSESSMENT GOALS, CRITERIA, and METHODOLOGY
The goals of nutrition assessment and therapy include prevention or reversal of nutrient deficiencies; preservation of lean body mass; increased tolerance for anticancer treatments with a minimization of nutrition-related side effects and complications; decreased risk for infection through support of immune function; facilitation of recovery and healing; and maintenance of strength, energy, and quality of life.
POTENTIAL RISK OF AGGRESSIVE NUTRITION THERAPY
Because weight loss and malnutrition are often significant in individuals fighting malignancy, clinical efforts frequency focus on increasing protein and energy intake by any means acceptable to patients, including use of the same type of cuisine that might have contributed to the initial development of the malignancy and that may be associated with poorer long-term survival. Although identification of nutrition problems and treatment of nutrition-related symptoms have been shown to stabilize or reverse weight loss in 50% to 88% of oncology patients, there is little evidence that these patients survive longer than patients whose weight loss is less aggressively treated. Evidence suggests that ad libitum diets high in fat, sugar, and animal protein may, by increasing cancer growth factors and stimulating cellular events leading to immune suppression and inflammation, foster cell proliferation and metastasis, interfere with effective treatment, and potentially worsen survival. These issues await further research.
Weight loss may lead to cachexia should be differentiated from healthful weight loss in overweight individuals. In certain cancers (eg, breast and colon), higher weight and/or greater percent body fat have been associated with increased mortality after diagnosis. One study of 526 individuals with colon cancer found that every 10% increase in body fat was associated with a 33% decrease in cancer survival. Caution should therefore be exercised in trying to prevent weight loss in individuals for whom such loss would otherwise be therapeutic, particularly in light of findings that adipocytes secrete adipocytokines (eg, leptin) that have an agonistic effect on cancer growth.
GASTROINTESTINAL DISTURBANCES
The National Cancer Institute and the American Cancer Society suggest the following dietary strategies to control the nausea and vomiting associated with chemotherapy.
- Eat prior to cancer treatments and have small, frequent meals
- Eat bland, soft, easy-to-digest foods rather than heavy meals
- Slowly sip fluids throughout the day
- Avoid foods that are likely to cause nausea. For some patients, these include spicy foods, greasy foods, and foods that have strong odors.
- Eat dry foods such as breadsticks, or toasts
- Sit up or lie with upper body raised for one hour after eating
- Avoid eating in a room that has cooking odors or that is overly warm. keep the living space at a comfortable temperature and with plenty of fresh air
- Rinse out the mouth before and after eating
- If these suggestions do not prevent vomiting, a clear liquid diet is suggested, with progression to a full liquid diet and then a soft diet (ie, bland foods that are softened by cooking, mashing, pureeing, or blending) as tolerated.
CONTROL OF DIARRHEA AND CONSTIPATION
For diarrhea, National Cancer Institute recommendations include consuming foods high in sodium and potassium (eg, broth, sports drinks, and bananas, peach and boiled or mashed potatoes) and bland, low-fiber foods (eg, rice, noodles, fruits, well-cooked vegetables), as well as avoiding very hot, cold, or caffeinated foods and beverages. Recommendations for constipation include a higher fiber (with physician approval, due to potentially undesirable effects in certain cancers), along with maintenance of physical activity and consumption of hot drink about half an hour before the usual time for a bowel movement, in the context of a high total fluid volume (at least 64 oz per day).
ANOREXIA
Suggestions provided by the National Cancer Institute for this condition are not geared toward its root causes but instead relate to strategies that may prevent its sequelae. These include planning menus in advance; eating frequent meals and snacks that are easy to prepare; adding liquid calorie sources (eg, juices, soups, and fruit smoothies); eating small frequent meals; seeking foods that appeal to the sense of smell; and experimenting in controlled trials.
RADIATION ENTERITIS
Symptoms of radiation enteritis include nausea, vomiting, abdominal cramping, tenesmus, and watery diarrhea. According to the NCI, a diet that is lactose-free, low in fat, and low in residue can be effective in symptom management. However, evidence supporting this approach is minimal and requires confirmation in controlled trials.
CHEMOTHERAPY-RELATED MUCOSITIS AND STOMATITIS
Practical dietary suggestions for dealing with this symptom include eating foods cold or at room temperature rather than warm or hot and eating soft foods that are easy to chew (eg, granola, toast, raw vegetables), or irritating (eg, spicy foods and citrus products). In patients treated with chemotherapy for a variety of cancers, oral glutamine supplementation was also found to decrease the incidence and severity of diarrhea, neuropathy, cardiotoxicity, and hepatic veno-occlusive disease that accompany the use of many chemotherapeutic agents.
HYPOGEUSIA
Blunted taste sensation often occurs in patients undergoing chemotherapy and radiation. it occurs in up to 70% of chemotheraoy-related patients and may contribute to lack of appetite and poor dietary intake, which, in turn, can worsen a patient's health status. Treatment with zinc sulfate (45 mg/day) reduces the occurrence of hypogeusia and speeds recovery of taste acuity in patients with head and neck cancer.
PREVENTION OF FOODBORNE ILLNESS DUE TO NEUTROPENIA
Avoidance of all possible sources of microbial contamination is suggested, including raw foods or those that cannot easily be decontaminated. In addition to the above considerations, some evidence supports the use of the following interventions:
For diarrhea, National Cancer Institute recommendations include consuming foods high in sodium and potassium (eg, broth, sports drinks, and bananas, peach and boiled or mashed potatoes) and bland, low-fiber foods (eg, rice, noodles, fruits, well-cooked vegetables), as well as avoiding very hot, cold, or caffeinated foods and beverages. Recommendations for constipation include a higher fiber (with physician approval, due to potentially undesirable effects in certain cancers), along with maintenance of physical activity and consumption of hot drink about half an hour before the usual time for a bowel movement, in the context of a high total fluid volume (at least 64 oz per day).
ANOREXIA
Suggestions provided by the National Cancer Institute for this condition are not geared toward its root causes but instead relate to strategies that may prevent its sequelae. These include planning menus in advance; eating frequent meals and snacks that are easy to prepare; adding liquid calorie sources (eg, juices, soups, and fruit smoothies); eating small frequent meals; seeking foods that appeal to the sense of smell; and experimenting in controlled trials.
RADIATION ENTERITIS
Symptoms of radiation enteritis include nausea, vomiting, abdominal cramping, tenesmus, and watery diarrhea. According to the NCI, a diet that is lactose-free, low in fat, and low in residue can be effective in symptom management. However, evidence supporting this approach is minimal and requires confirmation in controlled trials.
CHEMOTHERAPY-RELATED MUCOSITIS AND STOMATITIS
Practical dietary suggestions for dealing with this symptom include eating foods cold or at room temperature rather than warm or hot and eating soft foods that are easy to chew (eg, granola, toast, raw vegetables), or irritating (eg, spicy foods and citrus products). In patients treated with chemotherapy for a variety of cancers, oral glutamine supplementation was also found to decrease the incidence and severity of diarrhea, neuropathy, cardiotoxicity, and hepatic veno-occlusive disease that accompany the use of many chemotherapeutic agents.
HYPOGEUSIA
Blunted taste sensation often occurs in patients undergoing chemotherapy and radiation. it occurs in up to 70% of chemotheraoy-related patients and may contribute to lack of appetite and poor dietary intake, which, in turn, can worsen a patient's health status. Treatment with zinc sulfate (45 mg/day) reduces the occurrence of hypogeusia and speeds recovery of taste acuity in patients with head and neck cancer.
PREVENTION OF FOODBORNE ILLNESS DUE TO NEUTROPENIA
Avoidance of all possible sources of microbial contamination is suggested, including raw foods or those that cannot easily be decontaminated. In addition to the above considerations, some evidence supports the use of the following interventions:
- Selenium supplements. In women receiving chemotherapy for ovarian cancer, selenium supplementation (200 ug/d) significantly increased white blood cell count and decreased hair loss, abdominal pain, weakness, malaise, and loss of appetite in one study. Shot-term treatment with high doses of selenium (4000 ug/d) reduces toxicity and bone marrow suppression in cisplatin-treated patients.
- Specialized enteral formulas. In research studies, patients who received surgical treatment for gastric or head and neck cancers and were fed formulas containing arginine, glutamine, omega-3 fatty acids, or a combination of these had superior outcomes compared with patients receiving standards enteral formulas. The experimental group demonstrated higher levels of total and T lymphocytes, T helper and natural killer cells and significant reduction in postoperative infections and wound complications. However, further study is needed to confirm the superiority of specialized over standard formulas with respect to immune parameters and infection rates.
- Behavioral interventions. Published studies support the effectiveness of behavioral interventions for chemotherapy-related nausea and vomiting, including hypnosis, guided imagery, relaxation, and distraction. Studies suggest that diet changes may reduce the likelihood of recurrence or other poor outcomes for certain types of malignancy.
|
WARBURG EFFECT: Hallmark of Cancer
|
SUGAR AND CANCER
|
Breast Cancer
The incidence of breast cancer in men is about 1% of the rate in women. In both genders, the incidence increases with age. Most of the cancers are invasive at the time of diagnosis; only about 20% represent carcinoma in situ. More than 85% of the invasive tumors are infiltrating ductal carcinoma.
RISK FACTORS
Individuals in higher socioeconomic status (SES) categories generally have greater risk of developing breast cancer as high as double the incidence in comparison with the lowest SES.
AGE
Incidence increases sharply until age 45 to 50 years. Incidence continues to increase with age after menopause, but at a slower rate. the rate of increase in incidence stabilizes in later years and declines near age 80. Mean age at diagnosis is 65 years.
FAMILY HISTORY
Risk increases with an increasing number of first- or second-degree relatives with breast cancer history.
GENETIC FACTORS
The presence of BRCA1 or BRCA2 gene mutations increases breast cancer risk.
REPRODUCTIVE EVENTS
These include early menarche, late menopause, older age at first birth, nulliparity, and lower parity.
RADIATION EXPOSURE
Radiation exposure is one of the few exogenous factor that have been clearly demonstrated to increase breast cancer risk.
SHORTER DURATION OF BREAST-FEEDING
Several cohort and case-control studies show protective benefits of breast-feeding. A multinational case-control study of nearly 150,000 women showed a decreased risk of 4.3% for each year of breast-feeding and 7% for each pregnancy.
OBESITY
Elevated estrogen levels, presumably due to peripheral aromatization of androstenedione to 1-estrone in adipose tissue, may increase breast cancer risk in overweight postmenopausal women. Higher birth weight and greater weight gain are also associated with an increased risk. In contrast, excess body fat may be associated with decreased risk of premenopausal breast cancer.
RISK FACTORS
Individuals in higher socioeconomic status (SES) categories generally have greater risk of developing breast cancer as high as double the incidence in comparison with the lowest SES.
AGE
Incidence increases sharply until age 45 to 50 years. Incidence continues to increase with age after menopause, but at a slower rate. the rate of increase in incidence stabilizes in later years and declines near age 80. Mean age at diagnosis is 65 years.
FAMILY HISTORY
Risk increases with an increasing number of first- or second-degree relatives with breast cancer history.
GENETIC FACTORS
The presence of BRCA1 or BRCA2 gene mutations increases breast cancer risk.
REPRODUCTIVE EVENTS
These include early menarche, late menopause, older age at first birth, nulliparity, and lower parity.
RADIATION EXPOSURE
Radiation exposure is one of the few exogenous factor that have been clearly demonstrated to increase breast cancer risk.
SHORTER DURATION OF BREAST-FEEDING
Several cohort and case-control studies show protective benefits of breast-feeding. A multinational case-control study of nearly 150,000 women showed a decreased risk of 4.3% for each year of breast-feeding and 7% for each pregnancy.
OBESITY
Elevated estrogen levels, presumably due to peripheral aromatization of androstenedione to 1-estrone in adipose tissue, may increase breast cancer risk in overweight postmenopausal women. Higher birth weight and greater weight gain are also associated with an increased risk. In contrast, excess body fat may be associated with decreased risk of premenopausal breast cancer.
PHYSICAL INACTIVITY
Physically active women are less likely to develop breast cancer, compared with sedentary women. Exercise may decrease risk by reducing circulating estrogen and androgen concentrations. In the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial involving nearly 39,000 women, roughly 4 hours per week of exercise was associated with a >20% reduction in these women's risk for breast cancer, compared twith the risk for women reporting no physical ctivity. Some evidence indicates that exercise may impart this benefit regardless of hormone receptor subtype (ie, ER+/PR+, or ER-/PR-) or menopausal status.
Physically active women are less likely to develop breast cancer, compared with sedentary women. Exercise may decrease risk by reducing circulating estrogen and androgen concentrations. In the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial involving nearly 39,000 women, roughly 4 hours per week of exercise was associated with a >20% reduction in these women's risk for breast cancer, compared twith the risk for women reporting no physical ctivity. Some evidence indicates that exercise may impart this benefit regardless of hormone receptor subtype (ie, ER+/PR+, or ER-/PR-) or menopausal status.
HIGH ENDOGENOUS SERUM ESTROGEN CONCENTRATIONS
Women with higher concentrations of circulating estrogen have a higher risk of developing breast cancer. In a clinical trial with 7,705 women, those whose serum estradiol concentrations were in the highest quartile had twice the risk for invasive postmenopausal breast cancer, compared with women with lower estradiol concentrations.
Women with higher concentrations of circulating estrogen have a higher risk of developing breast cancer. In a clinical trial with 7,705 women, those whose serum estradiol concentrations were in the highest quartile had twice the risk for invasive postmenopausal breast cancer, compared with women with lower estradiol concentrations.
ELEVATED BLOOD GLUCOSE
The Nurses' Health Study found that post-menopausal women with diabetes had a slightly greatly risk for breast cancer. Other studies have found greater risk for breast cancer in non-diabetic women with higher level of fasting glucose.
INSUFFICIENT VITAMIN D
In a pooled analysis of two studies examining vitamin D and risk of breast cancer, women whose serum 25 (OH) D levels were in the lowest quantile (<13ng/dL) had twice the odds of developing breast cancer as those whose levels were in the highest quantile (>52 ng/dL.) An inverse dose-response relationship was detected, suggesting that the lower the circulating vitamin D level, the higher the risk of breast cancer. The authors reported that a level of 50 ng/dL could be achieved by oral intake of 2,000 IU of vitamin D3, coupled with moderate, regular sun exposure.
The Nurses' Health Study found that post-menopausal women with diabetes had a slightly greatly risk for breast cancer. Other studies have found greater risk for breast cancer in non-diabetic women with higher level of fasting glucose.
INSUFFICIENT VITAMIN D
In a pooled analysis of two studies examining vitamin D and risk of breast cancer, women whose serum 25 (OH) D levels were in the lowest quantile (<13ng/dL) had twice the odds of developing breast cancer as those whose levels were in the highest quantile (>52 ng/dL.) An inverse dose-response relationship was detected, suggesting that the lower the circulating vitamin D level, the higher the risk of breast cancer. The authors reported that a level of 50 ng/dL could be achieved by oral intake of 2,000 IU of vitamin D3, coupled with moderate, regular sun exposure.
Researchers have long noted the low incidence of breast cancer in countries where traditional diets based on plant foods prevail. A striking increase in breast cancer incidence has been noted in immigrants who have abandoned traditional diets (eg, rice, vegetables, soy foods) and adopted Western diets high in meat, dairy products, and fat. These observations have led scientists to hypothesize that diet-related factors, particularly obesity, play a key role in breast cancer risk. Part of this risk may be related to an increase in estrogen production from adipose tissue ad to eating fatty, low-fiber foods that maintain elevated circulating estrogen concentrations. Certain micronutrients, such as folate, that are commonly found in vegetables and fruits may also play a protective role. However, it may be that risk depends on dietary patterns, rather than on intake of individual foods and nutrients.
Although the group have not conducted randomized controlled trials on breast cancer, what affects prostate cancer may affect breast cancer as well. Lifestyle Medicine program downregulated oncogenes that promote breast cancer as well as prostate cancer and colon cancer in only three months. As with prostate cancer, it is likely that some aggressive breast cancers with high potential for spreading may require chemotherapy, surgery, and/or radiation whereas others may be safely treated with lifestyle medicine alone. Even when drugs and surgery are indicated, lifestyle medicine may add additional efficacy and reduce the likelihood of recurrence. For example, women who reduced their dietary fat intake to only 20 percent (about 33 grams of fat per day) decreased their risk of breast cancer recurrence by 42 percent after five years when compared with a randomized comparison group who consumed 51 grams of fat per day.
Although the group have not conducted randomized controlled trials on breast cancer, what affects prostate cancer may affect breast cancer as well. Lifestyle Medicine program downregulated oncogenes that promote breast cancer as well as prostate cancer and colon cancer in only three months. As with prostate cancer, it is likely that some aggressive breast cancers with high potential for spreading may require chemotherapy, surgery, and/or radiation whereas others may be safely treated with lifestyle medicine alone. Even when drugs and surgery are indicated, lifestyle medicine may add additional efficacy and reduce the likelihood of recurrence. For example, women who reduced their dietary fat intake to only 20 percent (about 33 grams of fat per day) decreased their risk of breast cancer recurrence by 42 percent after five years when compared with a randomized comparison group who consumed 51 grams of fat per day.
Alcohol
Alcohol intake is associated with a linear increase in incidence of breast cancer up to 5 drinks a day. Women who consumed 2 (approximately 30g ethanol) or more drinks per day had a relative risk of 1.41 compared with nondrinkers. Even 1 drink daily increases risk 9% to 10%. The risk is additive with HRT. Increased risk of breast cancer due to alcohol use may be mediated by the effect of sex hormone level. In 2010, the official World Health Organization body that assesses cancer risks formally upgraded its classification of alcohol to a definitive human breast carcinogen. In 2014, it clarified its position by stating that, regarding breast cancer, no amount of alcohol is safe.
But what about drinking “responsibly”? In 2013, scientists published a compilation of more than one hundred studies on breast cancer and light drinking (up to one alcoholic beverage a day). The researches had found a small but statistically significant increase in breast cancer risk even among women who had at most one drink per day (except, perhaps, for red wine see box below). They estimated that, every year around the world, nearly five thousand breast cancer deaths may be attributable to light drinking.
The carcinogen isn't alcohol itself. The culprit is actually the toxic breakdown product of alcohol called acetaldehyde, which can form in your mouth almost immediately after you take a sip. Experiments show that even holding single teaspoon of hard liquor in your mouth for five seconds before spitting out results in the production of potentially carcinogenic levels of acetaldehyde that lingers for more than ten minutes. If even a single sip of alcohol might produce cancer-causing levels of acetaldehyde in the mouth, what about using mouthwash that contains alcohol Researchers who tested the effects of a variety of retail mouthwashes and oral rinses concluded that, although the risk is slight, it is probably best to refrain from using such products if they contain alcohol.
Red Wine Versus White Wine
|
The Harvard Nurses' Health Study found that even less than one drink a day may be associated with a small increase in breast cancer risk. Interestingly, drinking only red wine was not associated with breast cancer risk. Why? A compound in red wine appears to suppress the activity of an enzyme called estrogen synthase, which breast tumors can use to create estrogen to fuel their own growth.
|
This compound is found in the skin of the dark-purple grapes used to make red wine, which explains why white wine appears to provide no such benefit, since it's produced without the skin. The researchers concluded that red wine may "ameliorate the elevated breast cancer risk associated with alcohol intake. In other words, the grapes in red wine may help cancel out some of the cancer-causing effects of the alcohol. But you can reap the benefits without the risks associated with imbibing alcoholic beverages by simply drinking grape juice or, even better, eating the purple grapes themselves preferably ones with seeds, as they appear to be most effective at suppressing estrogen synthase.
Sleep and Breast Cancer
Conversely, women who interrupt their melatonin production by working night shifts appear to be at increased risk for breast cancer. Even living on a particularly brightly lit street may affect the risk. Studies comparing night-time satellite photos against breast cancer rates have found that people living in brighter neighborhoods tend to have a higher breast cancer risk. Therefore, it's probably best to sleep without any lights on and with the blinds down, though the evidence to support these strategies is limited.
Melatonin production can be gauged by measuring the amount of melatonin excreted in our first pee in the morning. And, indeed, women with higher melatonin secretion have been found to have lower rates of breast cancer. Other than minimizing night time light exposure, is there anything else you can do to keep up your production of melatonin? Apparently so. In 2005, Japanese researchers reported an association between higher vegetable intake and higher melatonin levels in the urine. Is there anything in your diet that may lower melatonin production, thereby potentially increasing breast cancer risk? We didn't know until a comprehensive study of diet and melatonin was published in 2009. Researchers at Harvard University asked nearly a thousand women about their consumption of thirty-eight different foods or food groups and measured their morning melatonin levels. Meat consumption was the only food significantly associated with lower melatonin production, for reasons that are yet unknown.
Minimizing melatonin disruption may therefore mean putting curtains on your windows, eating more vegetables, and lowering the curtain on eating too much meat.
Conversely, women who interrupt their melatonin production by working night shifts appear to be at increased risk for breast cancer. Even living on a particularly brightly lit street may affect the risk. Studies comparing night-time satellite photos against breast cancer rates have found that people living in brighter neighborhoods tend to have a higher breast cancer risk. Therefore, it's probably best to sleep without any lights on and with the blinds down, though the evidence to support these strategies is limited.
Melatonin production can be gauged by measuring the amount of melatonin excreted in our first pee in the morning. And, indeed, women with higher melatonin secretion have been found to have lower rates of breast cancer. Other than minimizing night time light exposure, is there anything else you can do to keep up your production of melatonin? Apparently so. In 2005, Japanese researchers reported an association between higher vegetable intake and higher melatonin levels in the urine. Is there anything in your diet that may lower melatonin production, thereby potentially increasing breast cancer risk? We didn't know until a comprehensive study of diet and melatonin was published in 2009. Researchers at Harvard University asked nearly a thousand women about their consumption of thirty-eight different foods or food groups and measured their morning melatonin levels. Meat consumption was the only food significantly associated with lower melatonin production, for reasons that are yet unknown.
Minimizing melatonin disruption may therefore mean putting curtains on your windows, eating more vegetables, and lowering the curtain on eating too much meat.
Exercise and Breast Cancer
|
Physical activity is considered a promising preventive measure against breast cancer" not only because it helps with weight control but because exercise tends to lower circulating estrogen levels. Five hours a week of vigorous aerobic exercise can lower estrogen and progesterone exposure by about 20 percent. But do you need to work out that long for it to be protective Although even light exercise is associated with lowered risk of some other types of cancer, for breast cancer, leisurely strolls don't
|
appear to cut it. Even an hour a day of activities such as slow dancing or light housework may not help. According to the largest study ever published on the subject, only women who worked up a sweat at least five or more times a week appeared to get significant protection." Moderately intensity activity may offer as much benefit as vigorous exercise, though. Walling at a moderate pace for an hour a day is considered a moderately intense level of exercise, but it wasn't put to the test until a 2013 study reported that, indeed, walking an hour a day or more is associated with significantly lower breast cancer risk.
Heterocyclic Amines
|
In 1939, a curious finding was published in a paper titled "Presence of Cancer-Producing Substances in Roasted Food." A researcher described how he could induce breast cancers in mice by painting their heads with extracts of roasted horse muscle. These "cancer-producing substances" have since been identified as heterocyclic amines (HCAs), described by the National Cancer Institute as "chemicals formed when muscle meat, including beef, pork, fish, and poultry, is cooked using high-temperature methods.
|
These cooking methods include roasting, pan frying, grilling, and baking. Eating boiled meat is probably the safest. People who eat meat that never goes above 212 degrees Fahrenheit produce urine and feces that are significantly less DNA damaging compared to those eating meat dry-cooked at higher temperatures. This means they have fewer mutagenic substances flowing through their bloodstreams and coming in contact with their colons. On the other hand, baking chicken for as few as fifteen minutes at about 350 degrees Fahrenheit leads to HCA production.
These carcinogens are formed in a high-temperature chemical reaction between some of the components of muscle tissue. (The lack of some of these substances in plants may explain why even fried veggie burgers don't contain measurable HCAs.)" The longer meat is cooked, the more HCAs form. This process may explain why eating well done meat is associated with increased risk of cancers of the breast, colon, esophagus, lung, pancreas, prostate, and stomach. The situation creates what the Harvard Health Letter called a meat preparation "paradox": Cooking meat thoroughly reduces the risk of contracting foodborne infections, but cooking meat too thoroughly may increase the risk of foodborne carcinogens.
Just because heterocyclic amines cause cancer in rodents doesn't mean they cause cancer in humans. In this case, though it turns out people may be even more susceptible. The livers of rodents have shown an uncanny ability to detoxify 99 percent of the HCAs scientists stuffed down the animals' throats (a technique known as gavage). But then, in 2008, researchers discovered that the livers of humans fed cooked chicken were only able to detoxify about half of these carcinogens, suggesting that the cancer risk is far higher than was previously thought based on experiments in rats.
The carcinogens found in cooked meat are thought to explain why, as the Long Island Breast Cancer Study Project reported in 2007, women who cat more grilled, barbecued, or smoked meats over their lifetimes may have as much as 47 percent higher odds of breast cancer. And the Lowa Women's Health Study found that women who ate their bacon, beefsteak, and burgers "very well done" had nearly five times the odds of getting breast cancer compared with women who preferred these meats served rare or medium.
To see what was happening inside the breast, researchers asked women undergoing breast-reduction surgery about their meat-cooking methods. The scientists were able to link the consumption of fried meat with the amount of DNA damage found within the women's breast tissue, the type of damage that can potentially cause a normal cell to mutate into a cancer cell. HCAs appear able both to initiate and to promote cancer growth. PhIP, one of the most abundant HCAs in cooked meat, was found to have potent estrogen-like effects, fueling human breast-cancer cell growth almost as powerfully as pure estrogen, on which most human breast tumors thrive. But that result was based on research in a petridish. How do we know that cooked-meat carcinogens find their way into human breast ducts, where most breast cancers arise? We didn't, until researchers measured the levels of PhIP in the breast milk of nonsmoking women. (HCAs are also found in cigarette smoke.) In this study, PhIP was found in the breast milk of women who ate meat at the same concentration known to significantly boost breast cancer cell growth.
No trace of PhIP was found in the breast milk of the one vegetarian participant. A similar finding was reported in a study comparing the levels of PhIP in people's hair. The chemical was detected in hair samples of all six of the meat eaters tested, but in only one of the six vegetarians (HCAs can also be found in fried eggs. Your body can rapidly rid itself of these toxins once exposure ceases. In fact, urine levels of PhIP can drop to zero within twenty-four hours of refraining from eating meat. So if you practice Meatless Mondays, the level of PhIP passing through your body may become undetectable by Tuesday morning. But diet is not the only source of PhIP. HCA levels in vegetarians who smoke may approach those of nonsmoking meat eaters. The heterocyclic amine PhIP is not just a so-called complete carcinogen, able to both initiate cancers and then promote their growth. PhIP may also then facilitate cancer spread.
Cancer develops in three major stages:
1) initiation the irreversible DNA damage that starts the process;
2) promotion, the growth and division of the initiated cell into a tumor; and
3) progression, which can involve the invasion of the tumor into surrounding tissue and metastasis (spread) to other areas of the body.
Scientists can test how invasive, or aggressive, a certain cancer is by putting its cells into an instrument called an invasion chamber. They place cancer cells on one side of a porous membrane and then gauge their ability to penetrate and spread through the membrane. When researchers placed metastatic breast cancer cells from a fifty-four-year-old woman in an invasion chamber all by themselves, relatively few were able to breach the barrier. But within seventy-two hours of adding PhIp to the chamber, the cancer cells became more invasive, crawling through the membrane at an accelerated rate.
PhIP in meat may therefore represent a three-strikes-you're-out type of carcinogen, potentially involved in every stage of breast cancer development. Staying away from the stuff isn't easy, though, eating the standard American diet. As the researchers note: Exposure to PhIP is difficult to avoid because of its presence in many commonly consumed cooked meats, particularly chicken, beef and fish.
Just because heterocyclic amines cause cancer in rodents doesn't mean they cause cancer in humans. In this case, though it turns out people may be even more susceptible. The livers of rodents have shown an uncanny ability to detoxify 99 percent of the HCAs scientists stuffed down the animals' throats (a technique known as gavage). But then, in 2008, researchers discovered that the livers of humans fed cooked chicken were only able to detoxify about half of these carcinogens, suggesting that the cancer risk is far higher than was previously thought based on experiments in rats.
The carcinogens found in cooked meat are thought to explain why, as the Long Island Breast Cancer Study Project reported in 2007, women who cat more grilled, barbecued, or smoked meats over their lifetimes may have as much as 47 percent higher odds of breast cancer. And the Lowa Women's Health Study found that women who ate their bacon, beefsteak, and burgers "very well done" had nearly five times the odds of getting breast cancer compared with women who preferred these meats served rare or medium.
To see what was happening inside the breast, researchers asked women undergoing breast-reduction surgery about their meat-cooking methods. The scientists were able to link the consumption of fried meat with the amount of DNA damage found within the women's breast tissue, the type of damage that can potentially cause a normal cell to mutate into a cancer cell. HCAs appear able both to initiate and to promote cancer growth. PhIP, one of the most abundant HCAs in cooked meat, was found to have potent estrogen-like effects, fueling human breast-cancer cell growth almost as powerfully as pure estrogen, on which most human breast tumors thrive. But that result was based on research in a petridish. How do we know that cooked-meat carcinogens find their way into human breast ducts, where most breast cancers arise? We didn't, until researchers measured the levels of PhIP in the breast milk of nonsmoking women. (HCAs are also found in cigarette smoke.) In this study, PhIP was found in the breast milk of women who ate meat at the same concentration known to significantly boost breast cancer cell growth.
No trace of PhIP was found in the breast milk of the one vegetarian participant. A similar finding was reported in a study comparing the levels of PhIP in people's hair. The chemical was detected in hair samples of all six of the meat eaters tested, but in only one of the six vegetarians (HCAs can also be found in fried eggs. Your body can rapidly rid itself of these toxins once exposure ceases. In fact, urine levels of PhIP can drop to zero within twenty-four hours of refraining from eating meat. So if you practice Meatless Mondays, the level of PhIP passing through your body may become undetectable by Tuesday morning. But diet is not the only source of PhIP. HCA levels in vegetarians who smoke may approach those of nonsmoking meat eaters. The heterocyclic amine PhIP is not just a so-called complete carcinogen, able to both initiate cancers and then promote their growth. PhIP may also then facilitate cancer spread.
Cancer develops in three major stages:
1) initiation the irreversible DNA damage that starts the process;
2) promotion, the growth and division of the initiated cell into a tumor; and
3) progression, which can involve the invasion of the tumor into surrounding tissue and metastasis (spread) to other areas of the body.
Scientists can test how invasive, or aggressive, a certain cancer is by putting its cells into an instrument called an invasion chamber. They place cancer cells on one side of a porous membrane and then gauge their ability to penetrate and spread through the membrane. When researchers placed metastatic breast cancer cells from a fifty-four-year-old woman in an invasion chamber all by themselves, relatively few were able to breach the barrier. But within seventy-two hours of adding PhIp to the chamber, the cancer cells became more invasive, crawling through the membrane at an accelerated rate.
PhIP in meat may therefore represent a three-strikes-you're-out type of carcinogen, potentially involved in every stage of breast cancer development. Staying away from the stuff isn't easy, though, eating the standard American diet. As the researchers note: Exposure to PhIP is difficult to avoid because of its presence in many commonly consumed cooked meats, particularly chicken, beef and fish.
Fiber and Breast Cancer
One of the reasons? Cholesterol may play a role in the development and progression of breast cancer. Cancer appears to feed on cholesterol. LDL cholesterol stimulates the growth of breast cancer cells in a petri dish they just gobble up the so-called bad cholesterol. Tumors may suck up so much cholesterol that cancer patients cholesterol levels tend to plummet as their cancer grows. This is not a good sign, as patient survival tends to be lowest when cholesterol uptake is highest.
The cancer is thought to be using the cholesterol to make estrogen or to shore up tumor membranes to help the cancer migrate and invade more tissue. In other words, breast tumors may take advantage of high circulating cholesterol levels to fuel and accelerate their own growth. Cancer's hunger for cholesterol is such that pharmaceutical companies have considered using LDL cholesterol as a Trojan horse to deliver antitumor drugs to cancer cells.
Though data have been mixed, the largest study on cholesterol and cancer to date including more than a million participants-found a 17 percent increased risk in women who had total cholesterol levels over 240 compared with women whose cholesterol was under 160. If lowering cholesterol may help lower breast cancer risk, what about taking cholesterol-lowering statin drugs? Statins looked promising in petri-dish studies, but population studies comparing breast cancer rates among statin users and nonusers showed inconsistent results. Some suggested statins decreased breast cancer risk, while others showed increased risk. Nearly all these studies were relatively short term, however. Most considered five years to be long-term statin use, but breast cancer can take decades to develop.
The first major study on the breast cancer risk of statin use for ten years or longer was published in 2013. It found that women who had been taking statins for a decade or more had twice the risk of both common types of infiltrating breast cancer: invasive ductal carcinoma and invasive lobular carcinoma. The cholesterol drugs doubled the risk. If confirmed, the public health implications of these findings are immense: Approximately one in four women in the United States over the age of forty-five may be taking these drugs. The number one killer of women is heart disease, not breast cancer, so women still need to bring down their cholesterol. You can likely achieve this without drugs by eating a healthy enough plant-based diet. And certain plant foods may be particularly protective.
Inadequate fiber consumption may also be a risk factor for breast cancer. Researchers at Yale University and elsewhere found that premenopausal women who ate more that about six grams of soluble fiber a day (the equivalent of about a single cup of black beans) had 62 percent lower odds of breast cancer compared with women who consumed less than around four grams a day. Fiber’s benefits appeared even more pronounced for estrogen-receptor-negative breast tumors, which are harder to treat: Premenopausal women on a higher fiber diet had 85 percent lower odds of that type of breast cancer.
How did the researchers arrive Hence, soluble fiber may be protective. The women in the study weren't getting their fiber from supplements, though; they were getting it from food. But this could mean that eating more fiber is merely evidence that the cancer-free women are eating more plant foods, the only place fiber is found naturally. Therefore, fiber itself might not be the active ingredient. Maybe there's something else protective in plant foods. "On the other hand," noted the researchers, "an increased consumption of fiber from foods of plant origin may reflect a reduced consumption of foods of animal origin. In other words, maybe it's not what they were eating more of but what they were eating less of.
The reason high fiber intake is associated with less breast cancer may be because of more beans or less bologna. Either way, an analysis of a dozen other breast cancer case-control studies reported similar findings, with lower breast cancer risk associated with indicators of fruit and vegetable intake, such as vitamin C intake, and higher breast cancer risk associated with higher saturated-fat intake an indicator of meat, dairy, and processed food intake). And according to these studies, the more whole plant foods you eat, the better it is for your health: Every twenty grams of fiber intake per day was associated with a 15 percent lower risk of breast cancer.
One problem with case-control studies, though, is that they rely on people's memory of what they've been eating, potentially introducing what's known as "recall bias." For example, if people with cancer are more likely to selectively remember more of the unhealthy things they ate, this skewed recall could artificially inflate the correlation between eating certain foods and cancer. Prospective cohort studies avoid this problem by following a group (cohort) of healthy women and their diets forward (prospectively) in time to see who gets cancer and who doesn't. A compilation of ten such prospective cohort studies on breast cancer and fiber intake came up with similar results to the dozen case-control studies mentioned above, a 14 percent lower risk of breast cancer for every twenty grams of fiber intake per day. The relationship between more fiber and less breast cancer may not be a straight line, though.
Breast cancer risk may not significantly fall until at least twenty-five grams of fiber a day is reached. Unfortunately, the average American woman appears to eat less than fifteen grams of fiber per day-only about half the minimum daily recommendation. Even the average vegetarian in the United States may only get about twenty grams daily. Healthier vegetarians, though, may average thirty-seven grams a day, and vegans forty-six grams daily." Meanwhile, the whole-food, plant-based diets used therapeutically to reverse chronic disease contain upward of sixty grams of fiber.
The cancer is thought to be using the cholesterol to make estrogen or to shore up tumor membranes to help the cancer migrate and invade more tissue. In other words, breast tumors may take advantage of high circulating cholesterol levels to fuel and accelerate their own growth. Cancer's hunger for cholesterol is such that pharmaceutical companies have considered using LDL cholesterol as a Trojan horse to deliver antitumor drugs to cancer cells.
Though data have been mixed, the largest study on cholesterol and cancer to date including more than a million participants-found a 17 percent increased risk in women who had total cholesterol levels over 240 compared with women whose cholesterol was under 160. If lowering cholesterol may help lower breast cancer risk, what about taking cholesterol-lowering statin drugs? Statins looked promising in petri-dish studies, but population studies comparing breast cancer rates among statin users and nonusers showed inconsistent results. Some suggested statins decreased breast cancer risk, while others showed increased risk. Nearly all these studies were relatively short term, however. Most considered five years to be long-term statin use, but breast cancer can take decades to develop.
The first major study on the breast cancer risk of statin use for ten years or longer was published in 2013. It found that women who had been taking statins for a decade or more had twice the risk of both common types of infiltrating breast cancer: invasive ductal carcinoma and invasive lobular carcinoma. The cholesterol drugs doubled the risk. If confirmed, the public health implications of these findings are immense: Approximately one in four women in the United States over the age of forty-five may be taking these drugs. The number one killer of women is heart disease, not breast cancer, so women still need to bring down their cholesterol. You can likely achieve this without drugs by eating a healthy enough plant-based diet. And certain plant foods may be particularly protective.
Inadequate fiber consumption may also be a risk factor for breast cancer. Researchers at Yale University and elsewhere found that premenopausal women who ate more that about six grams of soluble fiber a day (the equivalent of about a single cup of black beans) had 62 percent lower odds of breast cancer compared with women who consumed less than around four grams a day. Fiber’s benefits appeared even more pronounced for estrogen-receptor-negative breast tumors, which are harder to treat: Premenopausal women on a higher fiber diet had 85 percent lower odds of that type of breast cancer.
How did the researchers arrive Hence, soluble fiber may be protective. The women in the study weren't getting their fiber from supplements, though; they were getting it from food. But this could mean that eating more fiber is merely evidence that the cancer-free women are eating more plant foods, the only place fiber is found naturally. Therefore, fiber itself might not be the active ingredient. Maybe there's something else protective in plant foods. "On the other hand," noted the researchers, "an increased consumption of fiber from foods of plant origin may reflect a reduced consumption of foods of animal origin. In other words, maybe it's not what they were eating more of but what they were eating less of.
The reason high fiber intake is associated with less breast cancer may be because of more beans or less bologna. Either way, an analysis of a dozen other breast cancer case-control studies reported similar findings, with lower breast cancer risk associated with indicators of fruit and vegetable intake, such as vitamin C intake, and higher breast cancer risk associated with higher saturated-fat intake an indicator of meat, dairy, and processed food intake). And according to these studies, the more whole plant foods you eat, the better it is for your health: Every twenty grams of fiber intake per day was associated with a 15 percent lower risk of breast cancer.
One problem with case-control studies, though, is that they rely on people's memory of what they've been eating, potentially introducing what's known as "recall bias." For example, if people with cancer are more likely to selectively remember more of the unhealthy things they ate, this skewed recall could artificially inflate the correlation between eating certain foods and cancer. Prospective cohort studies avoid this problem by following a group (cohort) of healthy women and their diets forward (prospectively) in time to see who gets cancer and who doesn't. A compilation of ten such prospective cohort studies on breast cancer and fiber intake came up with similar results to the dozen case-control studies mentioned above, a 14 percent lower risk of breast cancer for every twenty grams of fiber intake per day. The relationship between more fiber and less breast cancer may not be a straight line, though.
Breast cancer risk may not significantly fall until at least twenty-five grams of fiber a day is reached. Unfortunately, the average American woman appears to eat less than fifteen grams of fiber per day-only about half the minimum daily recommendation. Even the average vegetarian in the United States may only get about twenty grams daily. Healthier vegetarians, though, may average thirty-seven grams a day, and vegans forty-six grams daily." Meanwhile, the whole-food, plant-based diets used therapeutically to reverse chronic disease contain upward of sixty grams of fiber.
Flaxeeds and Breast Cancer
|
Flaxseeds are one of the first items ever considered to be health foods, treasured for their purported healing properties since at least the times of ancient Greece, when the renowned physician Hippocrates wrote about using them to treat patients. Better known as one of the richest plant sources of essential omega-3 fatty acids, flaxseeds are really set apart by their lignan content.
|
Though lignans are found throughout the plant kingdom, flaxseeds have around one hundred times more lignans than other foods. What are lignans? Lignans are phytoestrogens that can dampen the effects of the body's own estrogen. This is why flaxseeds are considered a first-line medical therapy for menstrual breast pain. In terms of breast cancer risk, eating about a daily tablespoonful of ground flaxseeds can extend a woman's menstrual cycle by about a day. This means she'll have fewer periods over the course of a lifetime and, therefore, presumably less estrogen exposure and reduced breast cancer risk. Just as broccoli doesn't technically contain sulforaphane (only the precursors that turn into sulforaphane when chewed), flaxseeds don't contain lignans, only lignan precursors, which need to be activated. This task is performed by the good bacteria in your gut.
The gut bacteria's role may help explain why women with frequent urinary tract infections may be at a higher risk of breast cancer: Every course of antibiotics you take can kill bacteria indiscriminately, meaning it may hinder the ability of the good bacteria in your gut to take full advantage of the lignans in your diet. (Yet another reason you should take antibiotics only when necessary.)
Lignan intake is associated with significantly reduced breast cancer risk in postmenopausal women. This effect is presumed to be due to lignans' further estrogen-dampening effects. But since lignans are found in healthy foods like berries, whole grains, and dark, leafy greens, could they just be an indicator of a healthy diet?
In a petri dish, lignans do directly suppress the proliferation of breast cancer cells. But the strongest evidence to date that there really is something special about this class of phytonutrients comes from interventional trials, starting with a 2010 study funded by the National Cancer Institute, Researchers took about forty five women at high risk of breast cancer - meaning they had suspicious breast biopsies or had previously suffered from breast cancer-and gave them the equivalent of about two teaspoons of ground flaxseeds every day. Needle biopsies of breast tissue were taken before and after the yearlong study. The results: On average, the women had fewer precancerous changes in their breasts after the year of flax lignans than before they started. Eighty percent (thirty-six of forty-five) had a drop in their levels of Ki 67, a biomarker (indicator) of increased cell proliferation. This finding suggests that sprinkling a few spoonfuls of ground flaxseeds on your oatmeal or whatever you're eating throughout the day may reduce the risk of breast cancer.
What about women who already have breast cancer? Breast cancer survivors who have higher levels of lignans in their bloodstreams and diets appear to survive significantly longer. This outcome may be due to the fact that women who eat flaxseeds may also see a rise in the levels of endostatin in their breasts. (Endostatin is a protein produced by your body to help starve tumors of their blood supply.)
The evidence from studies like these appeared so compelling that scientists performed a randomized, double-blind, placebo-controlled clinical trial of flaxseeds for breast cancer patients one of the few times a food has ever been so rigorously put to the test. Researchers located women with breast cancer scheduled for surgery and divided them randomly into two groups: Every day, group one ate a muffin containing flaxseed, while group two ate a muffin that looked and tasted the same, but had no flaxseed in it. Biopsies of the tumors in the flax and no-flax groups were taken at the beginning of the study and then compared with the pathology of the tumor removed during surgery about five weeks later.
Was there any difference? Compared with the women who ate the placebo muffins, women consuming the muffins with flaxseed, on average, witnessed their tumor-cell proliferation decrease, cancer cell death rates increase, and their C-erB2 scores go down. C-erB2 is a marker of cancer aggressiveness; the higher your score, the higher the potential for breast cancer to metastasize and spread throughout the body. In other words, the flaxseeds appeared to make the subjects' cancer less aggressive. The researchers concluded, “Dietary flaxseed has the potential to reduce tumor growth in patients with breast cancer. Flaxseed, which is inexpensive and readily available, may be a potential dietary alternative or adjunct to currently used breast cancer drugs."
The gut bacteria's role may help explain why women with frequent urinary tract infections may be at a higher risk of breast cancer: Every course of antibiotics you take can kill bacteria indiscriminately, meaning it may hinder the ability of the good bacteria in your gut to take full advantage of the lignans in your diet. (Yet another reason you should take antibiotics only when necessary.)
Lignan intake is associated with significantly reduced breast cancer risk in postmenopausal women. This effect is presumed to be due to lignans' further estrogen-dampening effects. But since lignans are found in healthy foods like berries, whole grains, and dark, leafy greens, could they just be an indicator of a healthy diet?
In a petri dish, lignans do directly suppress the proliferation of breast cancer cells. But the strongest evidence to date that there really is something special about this class of phytonutrients comes from interventional trials, starting with a 2010 study funded by the National Cancer Institute, Researchers took about forty five women at high risk of breast cancer - meaning they had suspicious breast biopsies or had previously suffered from breast cancer-and gave them the equivalent of about two teaspoons of ground flaxseeds every day. Needle biopsies of breast tissue were taken before and after the yearlong study. The results: On average, the women had fewer precancerous changes in their breasts after the year of flax lignans than before they started. Eighty percent (thirty-six of forty-five) had a drop in their levels of Ki 67, a biomarker (indicator) of increased cell proliferation. This finding suggests that sprinkling a few spoonfuls of ground flaxseeds on your oatmeal or whatever you're eating throughout the day may reduce the risk of breast cancer.
What about women who already have breast cancer? Breast cancer survivors who have higher levels of lignans in their bloodstreams and diets appear to survive significantly longer. This outcome may be due to the fact that women who eat flaxseeds may also see a rise in the levels of endostatin in their breasts. (Endostatin is a protein produced by your body to help starve tumors of their blood supply.)
The evidence from studies like these appeared so compelling that scientists performed a randomized, double-blind, placebo-controlled clinical trial of flaxseeds for breast cancer patients one of the few times a food has ever been so rigorously put to the test. Researchers located women with breast cancer scheduled for surgery and divided them randomly into two groups: Every day, group one ate a muffin containing flaxseed, while group two ate a muffin that looked and tasted the same, but had no flaxseed in it. Biopsies of the tumors in the flax and no-flax groups were taken at the beginning of the study and then compared with the pathology of the tumor removed during surgery about five weeks later.
Was there any difference? Compared with the women who ate the placebo muffins, women consuming the muffins with flaxseed, on average, witnessed their tumor-cell proliferation decrease, cancer cell death rates increase, and their C-erB2 scores go down. C-erB2 is a marker of cancer aggressiveness; the higher your score, the higher the potential for breast cancer to metastasize and spread throughout the body. In other words, the flaxseeds appeared to make the subjects' cancer less aggressive. The researchers concluded, “Dietary flaxseed has the potential to reduce tumor growth in patients with breast cancer. Flaxseed, which is inexpensive and readily available, may be a potential dietary alternative or adjunct to currently used breast cancer drugs."
Soy and Breast Cancer
|
Soybeans naturally contain another class of phytoestrogens called isoflavones. People hear the word "estrogen" in the word "phytoestrogens" and assume that means soy has estrogen-like effects. Not necessarily. Phytoestrogens dock into the same receptors as your own estrogen but have a weaker effect, so they can act to block the effects of your more powerful animal estrogen.
|
There are two types of estrogen receptors in the body, alpha and beta. Your own estrogen prefers alpha receptors, while plant estrogens (phytoestrogens) have an affinity for the beta receptors. The effects of soy phytoestrogens on different tissues therefore depend on the ratio of alpha to beta receptors. Estrogen has positive effects in some tissues and potentially negative effects in others. For example, high levels of estrogen can be good for the bones but can increase the likelihood of developing breast cancer. Ideally, you'd like what's called a "selective estrogen receptor modulator" in your body that would have proestrogenic effects in some tissues and antiestrogenic effects in others.
Well, that's what soy phytoestrogens appear to be. Soy seems to lower breast cancer risk, an antiestrogenic effect, but can also help reduce menopausal hot-flash symptoms, a proestrogenic effect. So, by eating soy, you may be able to enjoy the best of both worlds.
What about soy for women with breast cancer? There have been five studies on breast cancer survivors and soy consumption. Overall, researchers have found that women diagnosed with breast cancer who ate the most soy lived significantly longer and had a significantly lower risk of breast cancer recurrence than those who ate less. The quantity of phytoestrogens found in just a single cup of soy milk may reduce the risk of breast cancer returning by percent. The improvement in survival for those eating more soy foods was found both in women whose tumors were responsive to estrogen (estrogen receptor-positive breast cancer) and those whose tumors were not (estrogen-receptor negative breast cancer). This also held true for both young women and older women. In one study, for example, 90 percent of the breast cancer patients who ate the most soy phytoestrogens after diagnosis were still alive five years later, while half of those who ate little to no soy were dead. One way soy may decrease cancer risk and improve survival is by helping to reactivate BRCA genes. BRCA1 and BRCA2 are so-called caretaker gene cancer-suppressing genes responsible for DNA repair. Mutations in this gene can cause a rare form of hereditary breast cancer. As has been well publicized, Angelina Jolie decided to undergo a preventive double mastectomy.
A National Breast Cancer Coalition survey found that the majority of women believe that most breast cancers occur among women with a family history or a genetic pre disposition to the disease. The reality is that as few as 2.5 percent of breast cancer cases are attributable to breast cancer running in the family. If the vast majority of breast cancer patients have fully functional BRCA genes, meaning that their DNA-repair mechanisms are intact, how did their breast cancer form, grow, and spread? Breast tumors appear able to suppress the expression of the gene through a process called methylation. While the gene itself is operational, the cancer has effectively turned it off or at least turned down its expression, potentially aiding the metastatic spread of a tumor. That's where soy may come in.
The isoflavones in soy appear to help turn BRCA protection back on, removing the methyl straitjacket the tumor tried to place on it. The dose breast cancer researchers used to achieve this result in vitro was pretty hefty, though the equivalent to eating about a cup of soybeans. Soy may also help women with variations of other breast cancer susceptibility genes known as MDM2 and CYP1B1. Women at increased genetic risk of breast cancer may therefore especially benefit from high soy intake. The bottom line is that no matter which genes you inherit, changes in your diet may be able to affect DNA expression at a genetic level, potentially boosting your ability to fight disease.
Well, that's what soy phytoestrogens appear to be. Soy seems to lower breast cancer risk, an antiestrogenic effect, but can also help reduce menopausal hot-flash symptoms, a proestrogenic effect. So, by eating soy, you may be able to enjoy the best of both worlds.
What about soy for women with breast cancer? There have been five studies on breast cancer survivors and soy consumption. Overall, researchers have found that women diagnosed with breast cancer who ate the most soy lived significantly longer and had a significantly lower risk of breast cancer recurrence than those who ate less. The quantity of phytoestrogens found in just a single cup of soy milk may reduce the risk of breast cancer returning by percent. The improvement in survival for those eating more soy foods was found both in women whose tumors were responsive to estrogen (estrogen receptor-positive breast cancer) and those whose tumors were not (estrogen-receptor negative breast cancer). This also held true for both young women and older women. In one study, for example, 90 percent of the breast cancer patients who ate the most soy phytoestrogens after diagnosis were still alive five years later, while half of those who ate little to no soy were dead. One way soy may decrease cancer risk and improve survival is by helping to reactivate BRCA genes. BRCA1 and BRCA2 are so-called caretaker gene cancer-suppressing genes responsible for DNA repair. Mutations in this gene can cause a rare form of hereditary breast cancer. As has been well publicized, Angelina Jolie decided to undergo a preventive double mastectomy.
A National Breast Cancer Coalition survey found that the majority of women believe that most breast cancers occur among women with a family history or a genetic pre disposition to the disease. The reality is that as few as 2.5 percent of breast cancer cases are attributable to breast cancer running in the family. If the vast majority of breast cancer patients have fully functional BRCA genes, meaning that their DNA-repair mechanisms are intact, how did their breast cancer form, grow, and spread? Breast tumors appear able to suppress the expression of the gene through a process called methylation. While the gene itself is operational, the cancer has effectively turned it off or at least turned down its expression, potentially aiding the metastatic spread of a tumor. That's where soy may come in.
The isoflavones in soy appear to help turn BRCA protection back on, removing the methyl straitjacket the tumor tried to place on it. The dose breast cancer researchers used to achieve this result in vitro was pretty hefty, though the equivalent to eating about a cup of soybeans. Soy may also help women with variations of other breast cancer susceptibility genes known as MDM2 and CYP1B1. Women at increased genetic risk of breast cancer may therefore especially benefit from high soy intake. The bottom line is that no matter which genes you inherit, changes in your diet may be able to affect DNA expression at a genetic level, potentially boosting your ability to fight disease.
Avoidance of Western Dietary Pattern
Diet in Western countries, high in meat and fat (particularly saturated and omega-6 fatty acids) and low in fruits, vegetables, legumes, whole grains, and fiber, are linked to higher breast cancer risk, although the specific aspects of this dietary pattern that account for this risk have not been clearly separated. Breast cancer is less prevalent in countries where diets are mainly plant-based, high in fruits, vegetables, grains, and legumes. Incidence increases successively in first-and second-generation immigrants to North America. Specific dietary factors under investigation for a potentially helpful role are described below, and it should be noted that research attention is focusing more on overall dietary patterns than on the effects of specific foods or single nutrients.
a. Limiting or avoiding meat. In the Nurses' Health Study II involving over 90,000 women, higher intakes of red meat (more than 5-7 servings week, compared with 3 or fewer servings/week) were associated with a 40% greater breast cancer risk in women with the more commonly diagnosed estrogen-receptor-positive / progesterone-receptor-positive breast cancer. Similarly, in the UK Women's Cohort Study involving more than 35,000 women, those consuming the most red meat (an average of 2 oz/d compared with none) had a roughly 40% greater risk for breast cancer. In this same study, a high intake of all processed meats (>20 g/d) was associated with an approximately 65% greater risk for postmenopausal breast cancer, compared with not eating processed meat. It is not yet clear whether these associations reflect the effect of meat-based diets on hormone concentrations, the presence of carcinogens (eg, heterocyclic amines, polycyclic aromatic hydrocarbons), or other factors.
a. Limiting or avoiding meat. In the Nurses' Health Study II involving over 90,000 women, higher intakes of red meat (more than 5-7 servings week, compared with 3 or fewer servings/week) were associated with a 40% greater breast cancer risk in women with the more commonly diagnosed estrogen-receptor-positive / progesterone-receptor-positive breast cancer. Similarly, in the UK Women's Cohort Study involving more than 35,000 women, those consuming the most red meat (an average of 2 oz/d compared with none) had a roughly 40% greater risk for breast cancer. In this same study, a high intake of all processed meats (>20 g/d) was associated with an approximately 65% greater risk for postmenopausal breast cancer, compared with not eating processed meat. It is not yet clear whether these associations reflect the effect of meat-based diets on hormone concentrations, the presence of carcinogens (eg, heterocyclic amines, polycyclic aromatic hydrocarbons), or other factors.
b. Reducing fat. The relationship between fat intake and breast cancer is controversial. Data from international correlational studies support an association between fat intake and breast cancer risk. Prospective studies within Western countries have been less convincing regarding a relationship between total fat intake and breast cancer risk, but some have indicted specific types of fat. In a 20-year follow-up study of more than 80,000 postmenopausal women in the Nurses' Health Study, neither the quantity nor specific type of fat intake in midlife was associated with greater breast cancer risk. In the Nurses' Health Study II involving more than 90,000 women, those in the highest quintile of fat intake had a slightly increased risk for premenopausal breast cancer, attributed mainly to the intake of high-fat dairy products and red meat. Similarly, the National Institutes of Health (NIH)-AARP Diet and Health Study involving nearly 189,000 women found that consumption of 40% of calories from fat was associated with a more than 30% greater risk for postmenopausal breast cancer, compared with eating half as much fat. Further analysis of subtype of fat consumed (ie, saturated, monounsaturated, polyunsaturated) indicated that only saturated fat was significantly associated with risk. High-fat diets (not just saturated fat) tend to promote weight gain, which may be associated with greater breast cancer risk. Increased adiposity leads to higher serum estrogen levels, which, in turn may also be associated with greater breast cancer risk. Dietary factors also influence the age of menarche, which can also increase life-time estrogen exposure. Animal fat and animal protein intake are also associated with elevated levels of insulin-like growth factor-1 (IGF-1). IGF-1 may, in turn, be associated with other established risk factors for breast cancer (eg, breast density).
Aside from reducing saturated fat intake, there may be benefit in reducing consumption of omega-6 fats (arachidonic acid, linoleic acid). A 2005 study showed that postmenopausal women with the highest vegetable oil intake (a common source of omega-6 fats), in comparison with those consuming the least, had more than double the risk for breast cancer. One presumptive mechanism, aside from a possible effect of fat on estrogen production, is an increase in formation of prostaglandin E. (an eicosanoid that triggers proliferation of tumor cells) through the cyclooxygenase (COX) enzyme. A role for this mechanism is supported by the fact that regular use of COX-inhibitory drugs (ASA and other NSAIDs) has been associated with a reduced breast cancer risk. The Women's Health Initiative (WHI) Dietary Modification Trial, which included 48,835 women, tested a diet that aimed to reduce fat intake to 20% of energy and to increase vegetable and fruit consumption. Selected participants were consuming more fat than the US average at study baseline. The actual fat intake achieved by study participants averaged 24% of energy at 1 year and drifted upward toward baseline values by the study's end. After 8.1 years of follow-up, breast cancer risk was 9% lower in the intervention group, compared with a control group, although this result did not reach statistical significance. One exception was for progesterone-receptor-negative tumors, for which the risk decreased by 24% (P=.001). While the study results fueled pessimism about the ability of dietary changes to significantly alter breast cancer risk, it should be noted that the intervention diet included much more fat, meat, and dairy products than the Asian diets associated with lower cancer risk.
c. High-fiber diets. Dietary fiber interrupts the enterohepatic circulation of estrogen by binding unconjugated estrogens in the gastrointestinal tract.60 High-fiber, low-fat diets reduce serum estradiol, which is known to be associated with breast cancer risk. A large study of postmenopausal women found that those eating the most fiber had the lowest risk for breast cancer. In this group risk was even lower among women eating the least fat. In addition to its influence on circulating estrogens, fiber has other physiologic effects that may reduce cancer risk. High-fiber diets help keep blood glucose levels within normal limits and lower the risk for adult-onset diabetes, both of which have been related to increased breast cancer risk.
d. Fruits, vegetables, and legumes. Fruits and vegetables have a number of bioactive components that may confer protection against breast cancer. Folate may be especially important in women who consume alcohol. Foods that contain folic acid (green leafy vegetables legumes, oranges) are likely to be more effective than folate supplements, due to the presence of other protective factors (eg, fiber, beta-carotene, vitamin C, and phytochemicals). The European Investigation into Cancer and Nutrition (EPIC) study concluded that fruit and vegetable intake was not related to breast cancer risk. However, a study that examined the risk for breast cancer in association with higher scoring on healthy dietary patterns (eg, the Alternate Healthy Eating Index, Recommended Food Score, or Alternate Mediterranean Diet) concluded that the vegetable component of these dietary patterns was protective against estrogen receptor-negative breast cancer. Consumption of legumes (including soy products) that are high in isoflavones and lignans is also associated with lower risk for breast cancer, an effect that is greater if intake of these foods begins before or during adolescence. A greater intake of isoflavones was also found to protect against breast cancer in a study of more than 21,000 native Japanese women, and a meta-analysis of epidemiologic studies indicated
a 30% lower risk for premenopausal women and a nearly 25% lower risk for postmenopausal women who consumed the most soy. Further evidence of the benefit of legumes and was noted in the Nurses' Health Study II, in which eating beans or lentils twice per week was associated with a 25% lower risk, compared with consuming those foods less than
once per month.
Survival After Diagnosis
The following considerations apply to recurrence and survival after diagnosis:
A. Lower body weight. Breast cancer patients with greater-than-average body weight experience a shortened survival time, and Japanese women who have less body fat are more likely to survive breast cancer. In the Nurses' Health Study, weight before diagnosis was positively associated with breast cancer recurrence and death. Even differences in body weight within or near the normal range may influence mortality. A Shanghai study of women previously treated for breast cancer showed that compared with women with a body mass index <23.0, mortality was higher in those with a body mass index of 23.0-24.99, and greater still among those with a body mass index of 25. Lower-fat diets. In Japan and certain other countries, age-adjusted death rates for breast cancer increased when high-fat foods (particularly butter and margarine, cheese, ham and sausage, and dairy products) became available. Prospective studies suggest that women consuming less fat at the time of diagnosis, and perhaps those who later alter their diets to reduce fat intake, have a better prognosis. Results from a large randomized clinical trial, the Women's Intervention Nutrition Study (WINS), showed that postmenopausal women previously treated for breast cancer who ate a low-fat diet were less likely to develop a recurrence or a new primary cancer, compared with those who ate a more typical diet. Risk of recurrence or new primary cancers was reduced by 24% for all breast cancers and by 42% for estrogen- receptor-negative cancers. Fruits and vegetables. Diets high in fruits and vegetables may enhance survival from breast cancer. The Women's Healthy Eating and Living (WHEL) study combined a low-fat diet with an additional emphasis on vegetables and fruits for postmenopausal women previously treated for breast cancer. The intervention was predicated on earlier observational studies that had detected associations of either body weight or diet composition with disease-free or overall survival. Women in the intervention group (an intensive arm fostering 5 daily vegetable servings plus 16 oz of vegetable juice; 3 fruit servings; 30 g of fiber, and 15% to 20% of energy intake from fat) of the WHEL study reduced serum concentrations of estradiol, bioavailable estradiol, estrone, and estrone sulfate. Within the comparison group (a less intensive arm fostering 5 fruit and vegetable servings per day), variations in carotenoid concentrations in the blood (a marker for vegetable and fruit intake) were inversely associated with risk of recurrence or new primary cancers. After follow-up for 5-11 years, those in the comparison group who consumed 5 or more daily servings of fruits and vegetables and engaged in an average of 30 minutes of walking 6 days per week had roughly half the mortality risk of those who either had less vegetable and fruit intake or who were less physically active. However, no differences were observed between the intervention and comparison groups with respect to either disease-free survival or overall survival, suggesting that increasing vegetable and fruit intake beyond 5 servings per day was not associated with further benefits.
More recent findings from the Long Island Breast Cancer Study Project involving more than 1200 women have also revealed a survival advantage with a change in diet. Women eating roughly 5-6 servings of fruits and vegetables per day had a roughly 25% lower all-cause mortality risk, compared with those consuming 0-2.5 daily servings. However this was not significant after adjustment for age and energy intake, and exercise was not considered as a variable. Part of the apparent benefit may be attributable to the combinations of carotenoids, folate, and phytochemicals present in these foods. In the National Breast Screening Study, a significantly lower risk of dying from breast cancer was observed with higher intakes of vitamin C and beta-carotene, 2 nutrients found in fruits and vegetables.
ORDERS
Aside from reducing saturated fat intake, there may be benefit in reducing consumption of omega-6 fats (arachidonic acid, linoleic acid). A 2005 study showed that postmenopausal women with the highest vegetable oil intake (a common source of omega-6 fats), in comparison with those consuming the least, had more than double the risk for breast cancer. One presumptive mechanism, aside from a possible effect of fat on estrogen production, is an increase in formation of prostaglandin E. (an eicosanoid that triggers proliferation of tumor cells) through the cyclooxygenase (COX) enzyme. A role for this mechanism is supported by the fact that regular use of COX-inhibitory drugs (ASA and other NSAIDs) has been associated with a reduced breast cancer risk. The Women's Health Initiative (WHI) Dietary Modification Trial, which included 48,835 women, tested a diet that aimed to reduce fat intake to 20% of energy and to increase vegetable and fruit consumption. Selected participants were consuming more fat than the US average at study baseline. The actual fat intake achieved by study participants averaged 24% of energy at 1 year and drifted upward toward baseline values by the study's end. After 8.1 years of follow-up, breast cancer risk was 9% lower in the intervention group, compared with a control group, although this result did not reach statistical significance. One exception was for progesterone-receptor-negative tumors, for which the risk decreased by 24% (P=.001). While the study results fueled pessimism about the ability of dietary changes to significantly alter breast cancer risk, it should be noted that the intervention diet included much more fat, meat, and dairy products than the Asian diets associated with lower cancer risk.
c. High-fiber diets. Dietary fiber interrupts the enterohepatic circulation of estrogen by binding unconjugated estrogens in the gastrointestinal tract.60 High-fiber, low-fat diets reduce serum estradiol, which is known to be associated with breast cancer risk. A large study of postmenopausal women found that those eating the most fiber had the lowest risk for breast cancer. In this group risk was even lower among women eating the least fat. In addition to its influence on circulating estrogens, fiber has other physiologic effects that may reduce cancer risk. High-fiber diets help keep blood glucose levels within normal limits and lower the risk for adult-onset diabetes, both of which have been related to increased breast cancer risk.
d. Fruits, vegetables, and legumes. Fruits and vegetables have a number of bioactive components that may confer protection against breast cancer. Folate may be especially important in women who consume alcohol. Foods that contain folic acid (green leafy vegetables legumes, oranges) are likely to be more effective than folate supplements, due to the presence of other protective factors (eg, fiber, beta-carotene, vitamin C, and phytochemicals). The European Investigation into Cancer and Nutrition (EPIC) study concluded that fruit and vegetable intake was not related to breast cancer risk. However, a study that examined the risk for breast cancer in association with higher scoring on healthy dietary patterns (eg, the Alternate Healthy Eating Index, Recommended Food Score, or Alternate Mediterranean Diet) concluded that the vegetable component of these dietary patterns was protective against estrogen receptor-negative breast cancer. Consumption of legumes (including soy products) that are high in isoflavones and lignans is also associated with lower risk for breast cancer, an effect that is greater if intake of these foods begins before or during adolescence. A greater intake of isoflavones was also found to protect against breast cancer in a study of more than 21,000 native Japanese women, and a meta-analysis of epidemiologic studies indicated
a 30% lower risk for premenopausal women and a nearly 25% lower risk for postmenopausal women who consumed the most soy. Further evidence of the benefit of legumes and was noted in the Nurses' Health Study II, in which eating beans or lentils twice per week was associated with a 25% lower risk, compared with consuming those foods less than
once per month.
Survival After Diagnosis
The following considerations apply to recurrence and survival after diagnosis:
A. Lower body weight. Breast cancer patients with greater-than-average body weight experience a shortened survival time, and Japanese women who have less body fat are more likely to survive breast cancer. In the Nurses' Health Study, weight before diagnosis was positively associated with breast cancer recurrence and death. Even differences in body weight within or near the normal range may influence mortality. A Shanghai study of women previously treated for breast cancer showed that compared with women with a body mass index <23.0, mortality was higher in those with a body mass index of 23.0-24.99, and greater still among those with a body mass index of 25. Lower-fat diets. In Japan and certain other countries, age-adjusted death rates for breast cancer increased when high-fat foods (particularly butter and margarine, cheese, ham and sausage, and dairy products) became available. Prospective studies suggest that women consuming less fat at the time of diagnosis, and perhaps those who later alter their diets to reduce fat intake, have a better prognosis. Results from a large randomized clinical trial, the Women's Intervention Nutrition Study (WINS), showed that postmenopausal women previously treated for breast cancer who ate a low-fat diet were less likely to develop a recurrence or a new primary cancer, compared with those who ate a more typical diet. Risk of recurrence or new primary cancers was reduced by 24% for all breast cancers and by 42% for estrogen- receptor-negative cancers. Fruits and vegetables. Diets high in fruits and vegetables may enhance survival from breast cancer. The Women's Healthy Eating and Living (WHEL) study combined a low-fat diet with an additional emphasis on vegetables and fruits for postmenopausal women previously treated for breast cancer. The intervention was predicated on earlier observational studies that had detected associations of either body weight or diet composition with disease-free or overall survival. Women in the intervention group (an intensive arm fostering 5 daily vegetable servings plus 16 oz of vegetable juice; 3 fruit servings; 30 g of fiber, and 15% to 20% of energy intake from fat) of the WHEL study reduced serum concentrations of estradiol, bioavailable estradiol, estrone, and estrone sulfate. Within the comparison group (a less intensive arm fostering 5 fruit and vegetable servings per day), variations in carotenoid concentrations in the blood (a marker for vegetable and fruit intake) were inversely associated with risk of recurrence or new primary cancers. After follow-up for 5-11 years, those in the comparison group who consumed 5 or more daily servings of fruits and vegetables and engaged in an average of 30 minutes of walking 6 days per week had roughly half the mortality risk of those who either had less vegetable and fruit intake or who were less physically active. However, no differences were observed between the intervention and comparison groups with respect to either disease-free survival or overall survival, suggesting that increasing vegetable and fruit intake beyond 5 servings per day was not associated with further benefits.
More recent findings from the Long Island Breast Cancer Study Project involving more than 1200 women have also revealed a survival advantage with a change in diet. Women eating roughly 5-6 servings of fruits and vegetables per day had a roughly 25% lower all-cause mortality risk, compared with those consuming 0-2.5 daily servings. However this was not significant after adjustment for age and energy intake, and exercise was not considered as a variable. Part of the apparent benefit may be attributable to the combinations of carotenoids, folate, and phytochemicals present in these foods. In the National Breast Screening Study, a significantly lower risk of dying from breast cancer was observed with higher intakes of vitamin C and beta-carotene, 2 nutrients found in fruits and vegetables.
ORDERS
- During active treatment, dietary orders should be written in consultation between the treating physician and a consulting dietitian.
- After treatment, a low-fat, vegetable-rich, plant-based diet.
- Exercise prescription (30 minutes per day of walking or equivalent energy expenditure).
- Alcohol cessation or minimization
Lifestyle Medicine and Prostate Cancer
Lifestyle medicine is better than radiation or surgery in treating most patients with early-stage prostate cancer. Prostate cancer is the most common cancer in men other than skin cancer. Most men, if they live long enough, will get prostate cancer even if it remains undiagnosed. Approximately one-third of men in their thirties or forties, one-half of men in their fifties and sixties, 70 percent of men in their seventies, and 80 percent of men in their eighties have prostate cancer even if they're not aware of it.
In other words, most men are going to die with prostate cancer, not from prostate cancer. Our immune system and other mechanisms keep it in check and it remains asymptomatic. What's increasingly well-documented is that the lifestyle choices you make each day have a major impact on whether or not you develop clinically significant prostate cancer. if your immune system is functioning effectively, then it can help keep prostate cancer from spreading - and prostate cancer is usually dangerous only when it spreads (metastasizes).
The importance of lifestyle medicine is even more relevant if you have biopsy-proven prostate cancer and want to reverse its progression. Many doctors were shocked when a major randomized controlled trial in the New England Journal of Medicine showed that after ten years, men diagnosed with early-stage prostate cancer who did nothing - called "watchful waiting" or "active surveillance" - lived as long as those who had surgery to remove their prostate or who underwent radiation treatments. Similar results were found in an earlier study.
Men who had surgery or radiation did have a lower rate of disease progression and metastases, but they were much more likely to become impotent, incontinent, or both - that is, maimed in the most personal ways - and they didn't live longer. Men who are diagnosed with early-stage prostate cancer often feel a tremendous pressure from themselves and from well-meaning friends and family to do something about the tumor growing in their prostate. So if the choice is between doing nothing and having radiation or surgery, most men choose the latter - even though it's unlikely to prolong their survival and very likely to reduce their quality of life.
Lifestyle medicine provides a third, better alternative. For guys who want a more macho way of putting it, let's call it "an aggressive, non-surgical, non-pharmacologic intervention." Dr. Dean Ornish and his colleagues conducted the first randomized controlled trial showing that lifestyle medicine program may slow, stop, or even reverse the progression of early-stage prostate cancer, without drugs or surgery. The study was done in collaboration with Dr. Peter Carroll (chair of urology at UCSF) and the late Dr. William Fair (when he was chief of urologic surgery and chair of urologic oncology at Memorial Sloan-Kettering Cancer Center).
There is a relatively small subset of men - approximately one out of forty-nine - who have especially aggressive forms of prostate cancer and may benefit from surgery or radiation. These tend to be men who are diagnosed with prostate cancer early in life, have rapidly rising prostate-specific antigen (PSA) levels, have Gleason scores greater than 6, have tumors that are located in an area more likely to spread, or have large tumors. Dr. Carroll has developed algorithms to help identify this subset of men. Even these men needing surgery or radiation may reduce the risk of recurrence by making these lifestyle changes after this procedure.
Other studies provide insight into why these lifestyle changes have such a powerful impact on the progression of prostate cancer. For example, researchers found that men who were diagnosed with prostate cancer who ate a diet higher in red and processed meat, high-fat dairy foods, and refined grains had a significantly higher risk of both prostate-cancer-related mortality and overall mortality compared with those who ate a whole-foods plant-based diet. They examined health and diet data from almost 1,000 men participating in the Physicians' health Study who were diagnosed with prostate cancer who were followed for an average of fourteen years after their diagnosis. Men who ate mostly Western diet had a 250 percent higher risk of prostate-cancer-related death - and a 67 percent increased risk of death from any cause. In contrast, men who ate mostly whole-foods plant-based diet had a 36 percent lower risk of death from all causes.
Of course, there is a time and place for high-tech medicine. We've all benefited form it. To be clear, drugs and surgery can be lifesaving in a crisis. And in the early stages of treating and reversing chronic diseases, drugs or surgery may be necessary in addition to intensive lifestyle changes, at least at the beginning while your body is healing. and some people may need drugs and/or surgery even when they make comprehensive lifestyle changes. Even then, though, we need to address the underlying causes - which are usually lifestyle related, and often treatable and even reversible with lifestyle medicine.
Prostate cancer is one of the most common malignancy in men. Although most cases progress slowly and may never become clinically apparent, the disease is the second-leading cause of death in men and the most common cause of cancer death in male nonsmokers. Further, because of the disease's strong association with age, the number of new cases and deaths from prostate cancer is expected to increase with the aging of the population. Nearly all prostate cancer cases are adenocarcinomas; less than 3% are transitional cell carcinomas. Hormonal factors are important in the etiology of prostate cancer. Research studies have shown strong associations with testosterone and insulin-like growth factor 1 (IGF-1). Symptoms often include dysuria, difficulty voiding, urinary frequency and retention, and hematuria. However, more than 80% of cases are asymptomatic and present with only an elevated prostate-specific antigen (PSA) level or firm nodule on digital rectal examination.
The most common sites of metastasis are lymph nodes and bone. A small number of cases present with symptoms of metastatic disease, such as vertebral back pain, renal failure due to ureteral obstruction, or weight loss.
RISK FACTORS
Age. Prevalence increases rapidly after middle age. The condition rarely occurs before age 45, whereas most men over 70 years show microscopic evidence of malignant cells.
Race. African American men have the highest incidence of and mortality from prostate cancer of any demographic group. They also tend to have higher serum PSA levels and more advanced disease at diagnosis.
Family history. Prostate cancer is likely influenced by several genetic factors. Men who have a first-degree relative with prostate cancer are twice as likely to develop the disease themselves. Early onset of prostate cancer in a first degree family member further increases the risk.
Genetics. A smaller number of CAG repeats in the gene coding for the androgen receptor has been associated with increased risk. The incidence of prostate cancer is higher in families with breast cancer, and patients with BRCA1 or BRCA2 mutations appear to have a 2-fold to 5-fold increased risk.
Obesity. In the Cancer Prevention Study II Nutrition Cohort that included 69,991 men, the risk for fatal prostate cancer was roughly 55% greater in men whose body mass indices (BMI) fell between 30 and 35, compared with men at a BMI below 25. In men treated with prostatectomy, obesity was also significantly associated with treatment failure.
Obesity-related diseases (eg, insulin resistance syndrome) appear to double the risk for prostate cancer.
High blood concentrations of IGF-I. IGF-I concentrations are aated with cancer risk and are influenced by both body weight and certain dietary intakes, as described in Nutritional Considerations below.
Lack of physical activity. In men aged 65 or older, a higher risk of advanced and fatal prostate cancer was found in those who were sedentary compared with those who were physically active. Other studies have concluded that a sedentary lifestyle is not associated with prostate cancer risk overall, but it may increase the risk for developing
aggressive prostate cancer.
NUTRITIONAL CONSIDERATIONS
Prostate cancer risk appears to be increasing worldwide, a trend that may be due in part to the globalization of Western eating habits. Prostate cancer risk has been associated with higher meat and dairy intake and with diets that are high in processed foods and low in fiber (including processed meat, red meat, refined grains and vegetable oils, and soft drinks). Conversely, evidence is accumulating that a low-fat, vegetarian diet may help prevent prostate cancer and possibly play a role in its treatment. The following principal issues have emerged in research on diet and prostate cancer.
Animal Products and Increased Risk
Populations consuming meat-based diets have higher risk of prostate cancer, compared with those following largely plant-based diets. In some studies, risk is associated with specific products or with a particular component of animal-derived products. For example, epidemiologic evidence suggests that prostate cancer risk increases with animal fat" or saturated fat intake. High intakes of red meat and dairy products were shown to be associated with twice the risk for metastatic prostate cancer compared with the lowest intakes. Not all studies have indicated strong associations between red meat and prostate cancer risk. Some have suggested that risk relates to processed meat only and that risk may be identified only in certain groups leg, black, rather than white, individuals.
Several mechanisms have been proposed to explain these associations;
Androgenic effects. High-fat, low-fiber diets are associated with elevated blood testosterone concentrations, presumably as a result of either increased production or decreased excretion. In turn, higher testosterone concentrations are associated with increased risk of prostate cancer. Men who adopt low-fat, high-fiber diets show about a 15% reduction in testosterone concentrations.
Insulin-like growth factor. The association between animal product intake and prostate cancer risk may also be mediated by insulin-like growth factor 1 (IGF-1), a peptide with hormonal actions that increases with animal fat and animal protein consumption.
Carcinogens produced by cooking. Carcinogenic heterocyclic amines and polycyclic aromatic hydrocarbons tend to form as meat is cooked at high temperatures, and these are associated with increased risk of prostate cancer.
Dairy Product Intake and Increased Risk
Dairy products may play a role in prostate cancer risk that is distinct from that of other animal products. Two large Harvard University Cohort studies (the Physicians' Health Study and the Health Professionals Follow-Up Study), among several other epidemiologic studies have shown significant increases in prostate cancer risk among the highest
consumers of dairy products, independent of fat content. Similarly, in the Alpha-Tocopherol, Beta-Carotene (ATBC) Cancer Prevention Study of 29,133 male smokers, the highest dairy consumers had a 26% higher risk compared with those consuming the least dairy products. Two mechanisms have been proposed to explain this association:
Additional Diet-Related Factors
In a study of men with high-grade prostatic intraepithelial neoplasia, lycopene supplementation (4 mg/d) was associated with a reduction in the number who developed occult prostate cancer, compared with a control group on low-lycopene diets.35 Lycopene may interfere with IGF-I and other mediators of prostate cancer risk, such as androgen signaling, oxidative stress, and interleukin-6.
Supplementation with lycopene has been associated with biochemical and clinical improvement in men with existing prostate cancer. However, caution regarding supplementation is warranted. Evidence indicates that other constituents of tomatoes, rather than lycopene alone, may be responsible for the apparent oncostatic effect seen in
humans in one small clinical trial. Additional studies are needed to determine the degree to which tomato products, lycopene, or both are useful for the prevention and treatment of prostate cancer.
Intake of cruciferous vegetables (eg, broccoli, cabbage, cauliflower, and Brussels sprouts) is also associated with reduced risk for prostate cancer, perhaps because these foods can induce phase Il detoxification enzymes, as well as cell-cycle arrest and apoptosis in prostate cancer cells.
Regular intake of allium vegetables (eg, onions, leeks, scallions, and garlic) has also been associated with a decreased risk of prostate cancer. In one study, allium vegetable intake was strongly associated with decreased prostate cancer mortality." In another study, risk of developing prostate cancer was 71% lower in daily consumers of onions, compared with nonconsumers. It has been suggested that the possible anticancer effects of allium vegetables may involve immune stimulation and resultant release of interleukin-2, tumor necrosis factor and interferon, and enhanced natural killer cell activity.
Selenium. In epidemiologic studies, men who consumed higher levels of selenium or had higher levels of selenium in their body tissues were about half as likely to develop prostate cancer, compared with those who had the lowest intakes." Preliminary data suggest that selenium supplements (200 pg/d) may reduce prostate cancer risk.
Alcohol. A large prospective cohort study found that alcohol was a minor factor in prostate cancer risk, except in men who tend to binge. Compared with abstainers, men who drank 105 grams of alcohol (equivalent to 8 to 9 drinks) or more per week but who drank only 1 to 2 days each week had a 60% higher risk.49 Although some evidence suggests that liquor consumption increases risk more than beer or wine, other evidence indicates that risk increases with any type of alcohol.
DIET AND PROGNOSIS
A limited number of studies have addressed diet's possible influence on survival after diagnosis. Overall, evidence suggests that low-fat, plant-based diets may be helpful. Observational studies show that higher saturated fat intakes are associated with a 3-fold higher prostate cancer mortality, compared with the lowest intake. Prospective studies have found an inverse association with monounsaturated fat intake. In the Health Professionals Follow-Up Study, prostate cancer patients with the highest intakes of tomato sauce had a 45% lower risk for disease progression, compared with individuals having the lowest intakes.
Limited evidence suggests a substantial improvement in prostate cancer survival with diets that emphasize whole grain, legumes, and vegetables and avoid dairy products and meats. In a small clinical trial, diet treatment increased PSA doubling time from 6.5 months to 17 months." Similarly, in a randomized clinical trial using a vegan diet and stress reduction in 93 men with early prostate cancer who had elected not to undergo other treatment, the intervention group experienced a mean PSA reduction of 4%, compared with a 6% increase in the control group. None of the experimental-group patients required medical treatment during the trial, but 6 control-group patients required conventional treatment, due to rising PSA concentrations or evidence of disease progression on magnetic resonance imaging.
Other investigators have found that a plant-based diet can significantly decrease the rate of PSA rise (or lead to a PSA reduction) in patients with recurrent prostate cancer. Growing evidence indicates that obese men treated for prostate cancer are at greater risk of recurrence compared with those nearer normal weight. As noted above, obesity (BMI 230 kg/m2) was significantly associated with treatment failure in one study. Studies also suggest that higher body mass index (BMI) is associated with more aggressive cancer progression (ie, high-grade disease, positive surgical margins, extraprostatic extension, and lymph node metastasis).
The benefits of a low-fat, plant-based diet and exercise take on particular significance in light of the fact that cardiovascular disease remains a leading cause of death in prostate cancer patients.
MILK AND PROSTATE CANCER
Since the U.S. National Dairy Board was first created by the Dairy and Tobacco Adjustment Act of 1983, it has spent more than $1 billion on advertising. By now, we're all familiar with its various slogans, such as "Milk is natural." But is it? Think about it. Humans are the only species who drink milk after weaning. It also does seem a bit unnatural to drink the milk of another species.
What about "Milk: It Does a Body Good"? All foods of animal origin contain sex steroid hormones, such as estrogen, but today's genetically "improved" dairy cows are milked throughout their pregnancies when their reproductive hormones are particularly high. These hormones naturally found even in organic cow's milk may play a role in the various associations identified between milk and other dairy products and hormone-related conditions, including acne, diminished male reproductive potential, and premature puberty. The hormone content in milk may explain why women who drink it appear to have five times the rate of twin births compared with women who do not drink milk. When it comes to cancer though, the greater concern may have to do with growth hormones.
Mother Nature designed cow's milk to put a few hundred pounds on a baby calf within a few months. A lifetime of human exposure to these growth factors in milk may help explain the connections found between dairy consumption and certain cancers. Leading Harvard University nutrition experts have expressed concern that the hormones in dairy products and other growth factors could stimulate the growth of hormone-sensitive tumors. Experimental evidence suggests that dairy could also promote the conversion of precancerous lesions or mutated cells into invasive cancers.
Concerns about milk and other dairy products first arose from population-scale date, such as the twenty-five-fold increase in prostate cancer in Japanese men since World War II, which coincided with a sevenfold increase in eff consumption, a ninefold increase in meat consumption, and twentyfold increase in dairy consumption. Though the rest of their diets remained comparatively stable and similar trends have been noted in other countries, there were myriad changes in Japanese society beyond eating more animal products that could have contributed to these rising cancer rates. So scientists took a closer look.
To control for as many variables as possible, researchers devised as experiment in which they dripped milk on human prostate cancer cells in a petri dish. The researchers chose organic cow's milk to exclude any effect of added hormones, such as the bovine growth hormone, which is commonly injected into conventionally raised cows so they produce more milk. The researchers found that cow's milk stimulated the growth of human prostate cancer cells in each of fourteen separate experiments, producing an average increase in cancer rates. So scientist took a closer look.
To control for as many variables as possible, researchers devised an experiment in which they dripped milk on human prostate cancer cells in a petri dish. The researchers chose organic cow's milk to exclude any effect of added hormones, such as the bovine growth hormone, which is commonly injected into conventionally raised cows so they produce more milk. The researchers found that cow's milk stimulated the growth of human prostate cancer cells in each of fourteen separate experiments, producing an average increase in cancer growth rate of more than 30 percent. In contrast, almond milk suppressed the growth of the cancer cells by more than 30 percent.
What happens in a petri dish, though, doesn't necessarily happen in people. Nevertheless, a compilation of case-control studies did coincide that cow's milk consumption is a risk factor for prostate cancer, and the same outcome was found for cohort studies. A 2015 meta-analysis found that high intakes of dairy products - milk, low-fat milk, cheese, but non dairy sources of calcium - appear to increase total prostate cancer risk.
EGGS, CHOLINE, AND CANCER
More than two million men are currently living with prostate cancer, but living with prostate cancer is better than dying from it. if the cancer is caught while still localized within the prostate, the chances of it killing you within the next five years are practically nil. However, if the cancer spreads far enough, your chances of surviving five years may be as low as one in three. For this reason, scientists have been desperate to identify factors involved in the spread of prostate cancer once it has emerged.
Hoping to identify possible culprits, Harvard University researchers recruited more than one thousand men with early-stage prostate cancer and followed them for several years. Compared with men who rarely ate eggs, men who ate even less than a single eff a day appeared to have twice the risk of prostate cancer progression, such as metastasizing into the bones. The only thing potentially worse for prostate cancer than eggs was poultry; Men with more aggressive cancer who regularly ate chicken and turkey had up to four times the risk of prostate cancer progression.
The researchers suggested that the link between consuming poultry and advancing cancer may be due to cooked-meat carcinogens (such as heterocyclic amines). For unknown reason, these carcinogens build up more in the muscles of chickens and turkeys than in those of other animals.
But what cancer-promoting substance is there in eggs? How could eating less than an egg a day double the risk of cancer invasion? The answer may be choline, a compound found concentrated in eggs. Higher levels of choline in the blood have been associated with increased risk of developing prostate cancer in the first place. This may explain the link between eggs and cancer progression. But what about cancer mortality? In a paper entitled "Choline Intake and Risk of Lethal Prostate Cancer," the same Harvard team found that men who consumed the most choline from food also had an increased risk of cancer death. Men who consumed two and a half or more eggs per week - basically an egg every three days - may have an 81 percent increased risk of dying from prostate cancer. The choline in eggs, like the carnitine in red meat, is converted into a toxin called trimethylamine by bacteria that exist in the guts of those who eat meat. And trimethylamine once oxidized in the liver, appears to increase the risk of heart attack, stroke and premature death.
In other words, most men are going to die with prostate cancer, not from prostate cancer. Our immune system and other mechanisms keep it in check and it remains asymptomatic. What's increasingly well-documented is that the lifestyle choices you make each day have a major impact on whether or not you develop clinically significant prostate cancer. if your immune system is functioning effectively, then it can help keep prostate cancer from spreading - and prostate cancer is usually dangerous only when it spreads (metastasizes).
The importance of lifestyle medicine is even more relevant if you have biopsy-proven prostate cancer and want to reverse its progression. Many doctors were shocked when a major randomized controlled trial in the New England Journal of Medicine showed that after ten years, men diagnosed with early-stage prostate cancer who did nothing - called "watchful waiting" or "active surveillance" - lived as long as those who had surgery to remove their prostate or who underwent radiation treatments. Similar results were found in an earlier study.
Men who had surgery or radiation did have a lower rate of disease progression and metastases, but they were much more likely to become impotent, incontinent, or both - that is, maimed in the most personal ways - and they didn't live longer. Men who are diagnosed with early-stage prostate cancer often feel a tremendous pressure from themselves and from well-meaning friends and family to do something about the tumor growing in their prostate. So if the choice is between doing nothing and having radiation or surgery, most men choose the latter - even though it's unlikely to prolong their survival and very likely to reduce their quality of life.
Lifestyle medicine provides a third, better alternative. For guys who want a more macho way of putting it, let's call it "an aggressive, non-surgical, non-pharmacologic intervention." Dr. Dean Ornish and his colleagues conducted the first randomized controlled trial showing that lifestyle medicine program may slow, stop, or even reverse the progression of early-stage prostate cancer, without drugs or surgery. The study was done in collaboration with Dr. Peter Carroll (chair of urology at UCSF) and the late Dr. William Fair (when he was chief of urologic surgery and chair of urologic oncology at Memorial Sloan-Kettering Cancer Center).
There is a relatively small subset of men - approximately one out of forty-nine - who have especially aggressive forms of prostate cancer and may benefit from surgery or radiation. These tend to be men who are diagnosed with prostate cancer early in life, have rapidly rising prostate-specific antigen (PSA) levels, have Gleason scores greater than 6, have tumors that are located in an area more likely to spread, or have large tumors. Dr. Carroll has developed algorithms to help identify this subset of men. Even these men needing surgery or radiation may reduce the risk of recurrence by making these lifestyle changes after this procedure.
Other studies provide insight into why these lifestyle changes have such a powerful impact on the progression of prostate cancer. For example, researchers found that men who were diagnosed with prostate cancer who ate a diet higher in red and processed meat, high-fat dairy foods, and refined grains had a significantly higher risk of both prostate-cancer-related mortality and overall mortality compared with those who ate a whole-foods plant-based diet. They examined health and diet data from almost 1,000 men participating in the Physicians' health Study who were diagnosed with prostate cancer who were followed for an average of fourteen years after their diagnosis. Men who ate mostly Western diet had a 250 percent higher risk of prostate-cancer-related death - and a 67 percent increased risk of death from any cause. In contrast, men who ate mostly whole-foods plant-based diet had a 36 percent lower risk of death from all causes.
Of course, there is a time and place for high-tech medicine. We've all benefited form it. To be clear, drugs and surgery can be lifesaving in a crisis. And in the early stages of treating and reversing chronic diseases, drugs or surgery may be necessary in addition to intensive lifestyle changes, at least at the beginning while your body is healing. and some people may need drugs and/or surgery even when they make comprehensive lifestyle changes. Even then, though, we need to address the underlying causes - which are usually lifestyle related, and often treatable and even reversible with lifestyle medicine.
Prostate cancer is one of the most common malignancy in men. Although most cases progress slowly and may never become clinically apparent, the disease is the second-leading cause of death in men and the most common cause of cancer death in male nonsmokers. Further, because of the disease's strong association with age, the number of new cases and deaths from prostate cancer is expected to increase with the aging of the population. Nearly all prostate cancer cases are adenocarcinomas; less than 3% are transitional cell carcinomas. Hormonal factors are important in the etiology of prostate cancer. Research studies have shown strong associations with testosterone and insulin-like growth factor 1 (IGF-1). Symptoms often include dysuria, difficulty voiding, urinary frequency and retention, and hematuria. However, more than 80% of cases are asymptomatic and present with only an elevated prostate-specific antigen (PSA) level or firm nodule on digital rectal examination.
The most common sites of metastasis are lymph nodes and bone. A small number of cases present with symptoms of metastatic disease, such as vertebral back pain, renal failure due to ureteral obstruction, or weight loss.
RISK FACTORS
Age. Prevalence increases rapidly after middle age. The condition rarely occurs before age 45, whereas most men over 70 years show microscopic evidence of malignant cells.
Race. African American men have the highest incidence of and mortality from prostate cancer of any demographic group. They also tend to have higher serum PSA levels and more advanced disease at diagnosis.
Family history. Prostate cancer is likely influenced by several genetic factors. Men who have a first-degree relative with prostate cancer are twice as likely to develop the disease themselves. Early onset of prostate cancer in a first degree family member further increases the risk.
Genetics. A smaller number of CAG repeats in the gene coding for the androgen receptor has been associated with increased risk. The incidence of prostate cancer is higher in families with breast cancer, and patients with BRCA1 or BRCA2 mutations appear to have a 2-fold to 5-fold increased risk.
Obesity. In the Cancer Prevention Study II Nutrition Cohort that included 69,991 men, the risk for fatal prostate cancer was roughly 55% greater in men whose body mass indices (BMI) fell between 30 and 35, compared with men at a BMI below 25. In men treated with prostatectomy, obesity was also significantly associated with treatment failure.
Obesity-related diseases (eg, insulin resistance syndrome) appear to double the risk for prostate cancer.
High blood concentrations of IGF-I. IGF-I concentrations are aated with cancer risk and are influenced by both body weight and certain dietary intakes, as described in Nutritional Considerations below.
Lack of physical activity. In men aged 65 or older, a higher risk of advanced and fatal prostate cancer was found in those who were sedentary compared with those who were physically active. Other studies have concluded that a sedentary lifestyle is not associated with prostate cancer risk overall, but it may increase the risk for developing
aggressive prostate cancer.
NUTRITIONAL CONSIDERATIONS
Prostate cancer risk appears to be increasing worldwide, a trend that may be due in part to the globalization of Western eating habits. Prostate cancer risk has been associated with higher meat and dairy intake and with diets that are high in processed foods and low in fiber (including processed meat, red meat, refined grains and vegetable oils, and soft drinks). Conversely, evidence is accumulating that a low-fat, vegetarian diet may help prevent prostate cancer and possibly play a role in its treatment. The following principal issues have emerged in research on diet and prostate cancer.
Animal Products and Increased Risk
Populations consuming meat-based diets have higher risk of prostate cancer, compared with those following largely plant-based diets. In some studies, risk is associated with specific products or with a particular component of animal-derived products. For example, epidemiologic evidence suggests that prostate cancer risk increases with animal fat" or saturated fat intake. High intakes of red meat and dairy products were shown to be associated with twice the risk for metastatic prostate cancer compared with the lowest intakes. Not all studies have indicated strong associations between red meat and prostate cancer risk. Some have suggested that risk relates to processed meat only and that risk may be identified only in certain groups leg, black, rather than white, individuals.
Several mechanisms have been proposed to explain these associations;
Androgenic effects. High-fat, low-fiber diets are associated with elevated blood testosterone concentrations, presumably as a result of either increased production or decreased excretion. In turn, higher testosterone concentrations are associated with increased risk of prostate cancer. Men who adopt low-fat, high-fiber diets show about a 15% reduction in testosterone concentrations.
Insulin-like growth factor. The association between animal product intake and prostate cancer risk may also be mediated by insulin-like growth factor 1 (IGF-1), a peptide with hormonal actions that increases with animal fat and animal protein consumption.
Carcinogens produced by cooking. Carcinogenic heterocyclic amines and polycyclic aromatic hydrocarbons tend to form as meat is cooked at high temperatures, and these are associated with increased risk of prostate cancer.
Dairy Product Intake and Increased Risk
Dairy products may play a role in prostate cancer risk that is distinct from that of other animal products. Two large Harvard University Cohort studies (the Physicians' Health Study and the Health Professionals Follow-Up Study), among several other epidemiologic studies have shown significant increases in prostate cancer risk among the highest
consumers of dairy products, independent of fat content. Similarly, in the Alpha-Tocopherol, Beta-Carotene (ATBC) Cancer Prevention Study of 29,133 male smokers, the highest dairy consumers had a 26% higher risk compared with those consuming the least dairy products. Two mechanisms have been proposed to explain this association:
- Hormonal effects of dairy products. Dairy products contain a variety of hormonally active compounds and may elevate blood concentrations of IGF-1.
- Calcium's ability to suppress vitamin D activation. Compared with men who have the lowest calcium intakes those with the highest intakes appear to have as much as double the risk for developing prostate cancer. In the Health Professionals Follow-Up Study of approximately 48,000 men, those with calcium intakes between 1500 and 1999 mg/d had an 85% greater risk, and those with intakes above 2,000 mg/d had a roughly 245% greater risk, compared with those who had calcium intakes between 500 and 749 mg/d. Not all studies, however, have shown an association between calcium and prostate cancer. The association between calcium and prostate cancer may be related calcium's tendency to suppress the activation of vitamin D from its hormone form. Among vitamin D's biological actions is maintenance of cellular differentiation within the prostate. In a sample of the Health Professionals Follow-Up Study cohort, higher calcium intake was associated with lower circulating 1,25(OH)2 vitamin D levels.
- Fruit and Vegetable Intake and Reduced Risk. Wish intake of certain fruits and vegetables is associated with reduced risk of prostate cancer. Lycopene is a carotenoid antioxidant that imparts a bright red color to tomatoes, watermelon, pink grapefruit, and other foods. Intake of lycopene-containing foods has been associated with a lower risk of prostate cancer 32,19 Not all studies support this finding, however. A prospective investigation involving over 29,000 subjects casts doubt on this association, with the possible exception of a protective effect in men with a family history of prostate cancer.34 Nevertheless, clinical trials have found evidence of benefit.
Additional Diet-Related Factors
In a study of men with high-grade prostatic intraepithelial neoplasia, lycopene supplementation (4 mg/d) was associated with a reduction in the number who developed occult prostate cancer, compared with a control group on low-lycopene diets.35 Lycopene may interfere with IGF-I and other mediators of prostate cancer risk, such as androgen signaling, oxidative stress, and interleukin-6.
Supplementation with lycopene has been associated with biochemical and clinical improvement in men with existing prostate cancer. However, caution regarding supplementation is warranted. Evidence indicates that other constituents of tomatoes, rather than lycopene alone, may be responsible for the apparent oncostatic effect seen in
humans in one small clinical trial. Additional studies are needed to determine the degree to which tomato products, lycopene, or both are useful for the prevention and treatment of prostate cancer.
Intake of cruciferous vegetables (eg, broccoli, cabbage, cauliflower, and Brussels sprouts) is also associated with reduced risk for prostate cancer, perhaps because these foods can induce phase Il detoxification enzymes, as well as cell-cycle arrest and apoptosis in prostate cancer cells.
Regular intake of allium vegetables (eg, onions, leeks, scallions, and garlic) has also been associated with a decreased risk of prostate cancer. In one study, allium vegetable intake was strongly associated with decreased prostate cancer mortality." In another study, risk of developing prostate cancer was 71% lower in daily consumers of onions, compared with nonconsumers. It has been suggested that the possible anticancer effects of allium vegetables may involve immune stimulation and resultant release of interleukin-2, tumor necrosis factor and interferon, and enhanced natural killer cell activity.
Selenium. In epidemiologic studies, men who consumed higher levels of selenium or had higher levels of selenium in their body tissues were about half as likely to develop prostate cancer, compared with those who had the lowest intakes." Preliminary data suggest that selenium supplements (200 pg/d) may reduce prostate cancer risk.
Alcohol. A large prospective cohort study found that alcohol was a minor factor in prostate cancer risk, except in men who tend to binge. Compared with abstainers, men who drank 105 grams of alcohol (equivalent to 8 to 9 drinks) or more per week but who drank only 1 to 2 days each week had a 60% higher risk.49 Although some evidence suggests that liquor consumption increases risk more than beer or wine, other evidence indicates that risk increases with any type of alcohol.
DIET AND PROGNOSIS
A limited number of studies have addressed diet's possible influence on survival after diagnosis. Overall, evidence suggests that low-fat, plant-based diets may be helpful. Observational studies show that higher saturated fat intakes are associated with a 3-fold higher prostate cancer mortality, compared with the lowest intake. Prospective studies have found an inverse association with monounsaturated fat intake. In the Health Professionals Follow-Up Study, prostate cancer patients with the highest intakes of tomato sauce had a 45% lower risk for disease progression, compared with individuals having the lowest intakes.
Limited evidence suggests a substantial improvement in prostate cancer survival with diets that emphasize whole grain, legumes, and vegetables and avoid dairy products and meats. In a small clinical trial, diet treatment increased PSA doubling time from 6.5 months to 17 months." Similarly, in a randomized clinical trial using a vegan diet and stress reduction in 93 men with early prostate cancer who had elected not to undergo other treatment, the intervention group experienced a mean PSA reduction of 4%, compared with a 6% increase in the control group. None of the experimental-group patients required medical treatment during the trial, but 6 control-group patients required conventional treatment, due to rising PSA concentrations or evidence of disease progression on magnetic resonance imaging.
Other investigators have found that a plant-based diet can significantly decrease the rate of PSA rise (or lead to a PSA reduction) in patients with recurrent prostate cancer. Growing evidence indicates that obese men treated for prostate cancer are at greater risk of recurrence compared with those nearer normal weight. As noted above, obesity (BMI 230 kg/m2) was significantly associated with treatment failure in one study. Studies also suggest that higher body mass index (BMI) is associated with more aggressive cancer progression (ie, high-grade disease, positive surgical margins, extraprostatic extension, and lymph node metastasis).
The benefits of a low-fat, plant-based diet and exercise take on particular significance in light of the fact that cardiovascular disease remains a leading cause of death in prostate cancer patients.
MILK AND PROSTATE CANCER
Since the U.S. National Dairy Board was first created by the Dairy and Tobacco Adjustment Act of 1983, it has spent more than $1 billion on advertising. By now, we're all familiar with its various slogans, such as "Milk is natural." But is it? Think about it. Humans are the only species who drink milk after weaning. It also does seem a bit unnatural to drink the milk of another species.
What about "Milk: It Does a Body Good"? All foods of animal origin contain sex steroid hormones, such as estrogen, but today's genetically "improved" dairy cows are milked throughout their pregnancies when their reproductive hormones are particularly high. These hormones naturally found even in organic cow's milk may play a role in the various associations identified between milk and other dairy products and hormone-related conditions, including acne, diminished male reproductive potential, and premature puberty. The hormone content in milk may explain why women who drink it appear to have five times the rate of twin births compared with women who do not drink milk. When it comes to cancer though, the greater concern may have to do with growth hormones.
Mother Nature designed cow's milk to put a few hundred pounds on a baby calf within a few months. A lifetime of human exposure to these growth factors in milk may help explain the connections found between dairy consumption and certain cancers. Leading Harvard University nutrition experts have expressed concern that the hormones in dairy products and other growth factors could stimulate the growth of hormone-sensitive tumors. Experimental evidence suggests that dairy could also promote the conversion of precancerous lesions or mutated cells into invasive cancers.
Concerns about milk and other dairy products first arose from population-scale date, such as the twenty-five-fold increase in prostate cancer in Japanese men since World War II, which coincided with a sevenfold increase in eff consumption, a ninefold increase in meat consumption, and twentyfold increase in dairy consumption. Though the rest of their diets remained comparatively stable and similar trends have been noted in other countries, there were myriad changes in Japanese society beyond eating more animal products that could have contributed to these rising cancer rates. So scientists took a closer look.
To control for as many variables as possible, researchers devised as experiment in which they dripped milk on human prostate cancer cells in a petri dish. The researchers chose organic cow's milk to exclude any effect of added hormones, such as the bovine growth hormone, which is commonly injected into conventionally raised cows so they produce more milk. The researchers found that cow's milk stimulated the growth of human prostate cancer cells in each of fourteen separate experiments, producing an average increase in cancer rates. So scientist took a closer look.
To control for as many variables as possible, researchers devised an experiment in which they dripped milk on human prostate cancer cells in a petri dish. The researchers chose organic cow's milk to exclude any effect of added hormones, such as the bovine growth hormone, which is commonly injected into conventionally raised cows so they produce more milk. The researchers found that cow's milk stimulated the growth of human prostate cancer cells in each of fourteen separate experiments, producing an average increase in cancer growth rate of more than 30 percent. In contrast, almond milk suppressed the growth of the cancer cells by more than 30 percent.
What happens in a petri dish, though, doesn't necessarily happen in people. Nevertheless, a compilation of case-control studies did coincide that cow's milk consumption is a risk factor for prostate cancer, and the same outcome was found for cohort studies. A 2015 meta-analysis found that high intakes of dairy products - milk, low-fat milk, cheese, but non dairy sources of calcium - appear to increase total prostate cancer risk.
EGGS, CHOLINE, AND CANCER
More than two million men are currently living with prostate cancer, but living with prostate cancer is better than dying from it. if the cancer is caught while still localized within the prostate, the chances of it killing you within the next five years are practically nil. However, if the cancer spreads far enough, your chances of surviving five years may be as low as one in three. For this reason, scientists have been desperate to identify factors involved in the spread of prostate cancer once it has emerged.
Hoping to identify possible culprits, Harvard University researchers recruited more than one thousand men with early-stage prostate cancer and followed them for several years. Compared with men who rarely ate eggs, men who ate even less than a single eff a day appeared to have twice the risk of prostate cancer progression, such as metastasizing into the bones. The only thing potentially worse for prostate cancer than eggs was poultry; Men with more aggressive cancer who regularly ate chicken and turkey had up to four times the risk of prostate cancer progression.
The researchers suggested that the link between consuming poultry and advancing cancer may be due to cooked-meat carcinogens (such as heterocyclic amines). For unknown reason, these carcinogens build up more in the muscles of chickens and turkeys than in those of other animals.
But what cancer-promoting substance is there in eggs? How could eating less than an egg a day double the risk of cancer invasion? The answer may be choline, a compound found concentrated in eggs. Higher levels of choline in the blood have been associated with increased risk of developing prostate cancer in the first place. This may explain the link between eggs and cancer progression. But what about cancer mortality? In a paper entitled "Choline Intake and Risk of Lethal Prostate Cancer," the same Harvard team found that men who consumed the most choline from food also had an increased risk of cancer death. Men who consumed two and a half or more eggs per week - basically an egg every three days - may have an 81 percent increased risk of dying from prostate cancer. The choline in eggs, like the carnitine in red meat, is converted into a toxin called trimethylamine by bacteria that exist in the guts of those who eat meat. And trimethylamine once oxidized in the liver, appears to increase the risk of heart attack, stroke and premature death.
|
|
|
Cancer of the Gastrointestinal System
Every year, Americans lose more than five million years of life from cancers that may have been prevented. Only a small percentage of all human cancers are attributable to purely genetic factors. The rest involve external factors, particularly our diet. Your skin covers about twenty square feet. Your lungs, if you were to flatten out all the tiny air pockets, could cover hundreds of square feet. And your intestines? Counting all the little folds, some scientists estimate that your gut would blanket thousands of square feet, vastly more expansive than your skin and lungs combined. What you eat may very well be your primary interface with the outside world. This means that regardless of the carcinogens that could be lurking in the environment, your greatest exposure may be through your diet.
Three of the most common cancers of the digestive tract kill approximately one hundred thousand Americans each year. Colorectal (colon and rectal) cancer, which claims fifty thousand lives annually, ranks among the most commonly diagnosed of all cancers. Thankfully, it is also among the most treatable if caught early enough. Pancreatic cancer, on the other hand, is virtually a death sentence for the approximately forty-six thousand people who develop it every year. Few survive beyond a year after diagnosis, which means prevention is paramount. Esophageal cancer, which affects the tube between your mouth and stomach, is also frequently fatal for its eighteen thousand annual victims. The foods you eat can indirectly affect cancer risk, for example, by exacerbating acid reflux, a risk factor for esophageal cancer, or through direct contact with the lining of the digestive tract.
COLORECTAL CANCER
The average person has about a one-in-twenty chance of developing colorectal cancer over the course of his or her lifetime. Fortunately, it is among the most treatable cancers, as regular screening has enabled doctors to detect and remove the cancer before it spreads. There are more than one million colorectal cancer survivors in the United States alone, and, among those diagnosed before the cancer has spread beyond the colon, the five-year survival rate is about 90 percent. But, in its early stages, colorectal cancer rarely causes symptoms. If the cancer is not caught until later stages, treatment is more difficult and less effective. Starting at age fifty until age seventy-five, you should either get stool testing every year, stool testing every three years plus a sigmoidoscopy every five years, or a colonoscopy every ten years. For more on the risks and benefits of these options. While regular screenings are certainly sensible to detect colorectal cancer, preventing it in the first place is even better.
TURMERIC
India's gross domestic product (GDP) is about eight times less than that of the United States," and about 20 percent of its population lives below the poverty line, yet cancer rates in India are much lower than in the United States. Women
in the United States may have ten times more colorectal cancer than women in India, seventeen times more lung cancer, nine times more endometrial cancer and melanoma, twelve times more kidney cancer, eight times more bladder cancer, and five times more breast cancer. Men in the United States appear to have eleven times more colorectal cancer than men in India, twenty-three times more prostate cancer, fourteen times more melanoma, nine times more kidney cancer, and seven times more lung and bladder cancer. Why such a discrepancy? The regular use of the spice turmeric in Indian cooking has been proposed as one possible explanation.
Curcumin, the yellow pigment in the spice turmeric, may be effective against cancer cells in vitro. Very little of the curcumin you eat gets absorbed into your bloodstream, however, so it may never come in sufficient contact with tumors outside the digestive tract. But what doesn't get absorbed into your blood ends up in your colon, where it could impact the cells lining your large intestine where cancerous polyps develop.
The emergence of colorectal cancer can be broken up into three stages. The first sign may be what are called "aberrant crypt foci, or abnormal clusters of cells along the lining of the colon. Next come polyps that grow from that inner surface. The final stage is thought to occur when a benign polyp transforms into a cancerous one. The cancer can then eat through the wall of the colon and spread throughout the body. To what degree can curcumin block each stage
of colorectal cancer?
Studying smokers, who tend to have a lot of aberrant crypt foci, investigators found that curcumin consumption could reduce the number of those cancer-associated structures in their rectums up to nearly 40 percent, from eighteen down to eleven, within just thirty days. The only reported side effect was a yellow tint to their stools. What if polyps have already developed? Six months of curcumin, along with another phytonutrient called quercetin, which is found naturally in such fruits and vegetables as red onions and grapes, were found to decrease the number and size of polyps by more than half in patients with a hereditary form of colorectal cancer. Again, virtually no side effects were reported."
What if the polyps have already transformed into cancer? In a last-ditch attempt to save the lives of fifteen patients with advanced colorectal cancer who didn't respond to any of the standard chemotherapy agents or radiation, oncologists started them on a turmeric extract. In the two to four months of treatment, it appeared to help stall the disease in one-third of the patients, five out of fifteen. If we were talking about some new kind of chemotherapy drug that only helped one in three people, you'd have to weigh that against all the serious side effects. But when it's just some plant extract shown to be remarkably safe, even if it just helped one in a hundred, it would be worth considering.
With no serious downsides, a one-in-three potential benefit for end-stage cancer seems like it would spark further research, right? But who's going to pay for a study of something that can't be patented? The low cancer rate in India may be due in part to the spices they use, but it may also stem from the types of foods they are putting those spices on. India is one of the world's largest producers of fruits and vegetables, and only about 7 percent of the adult population eats meat on a daily basis. What most of the population does eat every day are dark-green, leafy vegetables and legumes, such as beans, split peas, chickpeas, and lentils, which are packed with another class of cancer-fighting compounds called phytates.
STOOL SIZE MATTERS
The bigger and more frequent your bowel movements are, the healthier you may be. Based on a study of twenty-three populations across a dozen countries, the incidence of colon cancer appears to skyrocket as the average daily stool weight drops below about a half a pound. Populations dropping quarter pounders appear to have three times the rate of colon cancer. You can measure the weight of your stools with a simple bathroom scale. No, not that way-by weighing yourself before and after you "go." The link between stool size and colon cancer may be related to "intestinal transit time," the number of hours it takes for food to travel from mouth to toilet. The larger the stool, the quicker the transit time, as it's easier for your intestines to move things along. People don't realize you can have daily bowel movements and still effectively be constipated; what you're flushing today you may have eaten last week. How long it takes food to get from one end to the other can depend on gender and dietary habits. Food goes through men eating plant-based diets in just a day or two, but this transit time takes as long as five or more days among those eating more conventional diets. Women eating plant-based diets also average a day or two, but the average intestinal transit time in most women eating conventional diets may be four days. So you can be regular but four days late.
You can measure your own oral-anal transit time by eating some beets and noting when your stools turn pink. If that takes less than twenty-four to thirty-six hours, you're probably meeting the healthy half pound target. Constipation is the most common gastrointestinal complaint in the United States, leading to millions of doctor visits each year. But beyond just the discomfort, the straining associated with trying to pass small, firm stools may play a role in a host of health problems, including hiatal hernia, varicose veins, hemorrhoids, and painful conditions with names like anal fissure. Constipation can be considered a nutrient-deficiency disease, and that nutrient is fiber. Just as you can get scurvy if you don't get enough vitamin C, you can get constipation if you don't get enough fiber. Since fiber is found only in plant foods, it's no surprise that the more plants you eat, the less likely you are to be constipated. For example, a study comparing thousands of omnivores, vegetarians, and vegans found that those eating strictly plant-based diets are three times more likely to have daily bowel movements. Looks like vegans are just regular people.
PHYTATES
Colorectal cancer is the second-leading cause of cancer-related death in the United States and in some parts of the world, it's practically unheard of. The highest rates have been recorded in Connecticut, and the lowest in Kampala Uganda. Why is colorectal cancer so much more prevalent in Western cultures? Seeking answers to this question, renowned surgeon Denis Burkitt spent twenty-four years in Uganda. Many of the Ugandan hospitals Dr. Burkitt visited had never even seen a case of colon cancer." He eventually came to the conclusion that fiber intake was the key, as most Ugandans consumed diets centered around whole plant foods.
Subsequent research has suggested that dietary prevention of cancer may involve something other than just fiber. For instance, colorectal cancer rates are higher in Denmark than in Finland, yet Danes consume slightly more dietary fiber than Finns. What other protective compounds might explain the low cancer rates among plant-based populations? Well, fiber isn't the only thing found in whole plant foods that's missing from processed and animal-based foods. The answer might lie in natural compounds called phytates, which are found in the seeds of plants in other words, in all whole grains, beans, nuts, and seeds. Phytates have been shown to detoxify excess iron in the body, which otherwise can generate a particularly harmful kind of free radical called hydroxyl radicals. The standard American diet may therefore be a double whammy when it comes to colorectal cancer: Meat contains the type of iron (heme) particularly associated with colorectal cancer but lacks, as do refined plant foods, the phytates to extinguish these iron-forged free radicals.
For many years, phytates were maligned as inhibitors of mineral absorption, which is why you might have heard advice to roast, sprout, or soak your nuts to get rid of the phytates. In theory, this would allow you to absorb more minerals, such as calcium. This belief stemmed from a series of laboratory experiments on puppies from 1949 that suggested that phytates had a bone-softening, anti-calcifying effect, as well as from subsequent studies with similar findings on rats. But more recently, in light of actual human data, phytates image has undergone a complete makeover. Those who eat more high-phytate foods actually tend to have a greater bone mineral density, less bone loss, and fewer hip fractures. Phytates appear to protect bone in a manner similar to that of antiosteoporosis drugs like Fosamax, but without the risk of osteonecrosis (bone rot) of the jaw, a rare, potentially disfiguring side effect associated with that class of drugs.
Colorectal cancer is the second-leading cause of cancer-related death in the United States, and in some parts of the world, it's practically unheard of. The highest rates have been recorded in Connecticut, and the lowest in Kampala Uganda. Why is colorectal cancer so much more prevalent in Western cultures? Seeking answers to this question, renowned surgeon Denis Burkitt spent twenty-four years in Uganda. Many of the Ugandan hospitals Dr. Burkitt visited had never even seen a case of colon cancer. He eventually came to the conclusion that fiber intake was the key, as most Ugandans consumed diets centered around whole plant foods. Subsequent research has suggested that dietary prevention of cancer may involve something other than just fiber. For instance, colorectal cancer rates are higher in Denmark than in Finland, yet Denis consume slightly more dietary fiber than Finns. What other protective compounds might explain the low cancer rates among plant-based populations? Well, fiber isn't the only thing found in whole plant foods that's missing from processed and animal-based foods.
The answer might lie in natural compounds called phytates, which are found in the seeds of plants in other words, in all whole grains, beans, nuts, and seeds. Phytates have been shown to detoxify excess iron in the body, which otherwise can generate a particularly harmful kind of free radical called hydroxyl radicals. The standard American diet may therefore be a double whammy when it comes to colorectal cancer: Meat contains the type of iron (heme) particularly associated with colorectal cancer but lacks, as do refined plant foods, the phytates to extinguish these iron-forged free radicals.
For many years, phytates were maligned as inhibitors of mineral absorption, which is why you might have heard advice to roast, sprout, or soak your nuts to get rid of the phytates. In theory, this would allow you to absorb more minerals, such as calcium. This belief stemmed from a series of laboratory experiments on puppies from 1949 that suggested that phytates had a bone softening, anti calcifying effect, as well as from subsequent studies with similar findings on rats. But more recently, in light of actual human data, those who eat more high-phytate foods actually tend to have a greater bone mineral density, less bone loss, and fewer hip fractures. Phytates appear to protect bone in a manner similar to that of antiosteoporosis drugs like Fosamax, but without the risk of osteonecrosis (bone rot) of the jaw, a rare, potentially disfiguring side effect associated with that class of drugs.
Phytates may also help protect against colorectal cancer. A six-year study of about thirty thousand Californians found that higher meat consumption was associated with higher risk of colon cancer. Unexpectedly, white meat appeared to be worse. Indeed, those who ate red meat at least once each week had about double the risk of developing colon cancer; that risk appeared to triple, however, for those who ate chicken or fish once or more a week. Eating beans, an excellent source of phytates, was found to help mediate some of that risk, so your colon cancer risk may be determined by your meat-to-vegetable ratio. There may be as much as an eightfold difference in colorectal cancer risk between the two extremes-high-vegetable, low-meat diets and low-vegetable, high-meat diets. So it may not be enough to just cut down on how much meat is in your diet; you also need to eat more plants.
The National Cancer Institute's Polyp Prevention Trial found that those who increased their bean consumption by even less than one-quarter cup a day appeared to cut their odds of precancerous colorectal polyp recurrence by up to 65 percent. Of all the wonderful nutrients in beans, why do we credit the phytates with reduced risk? Petri-dish studies have shown that phytates inhibit the growth of virtually all human cancer cells tested so far-including cancers of the colon, breast, cervix, prostate, liver, pancreas, and skin while leaving normal cells alone. This is the mark of a good anticancer agent, the ability to discriminate between tumor cells and normal tissue. When you eat whole grains, beans, nuts, and seeds, phytates are rapidly absorbed into the bloodstream and readily taken up by tumor cells. Tumors concentrate these compounds so efficiently that phytate scans can be used to trace the spread of cancer within the body.
Phytates target cancer cells through a combination of antioxidant, anti-inflammatory, and immune-enhancing activities. Besides affecting the cancer cells directly, phytates have been found to boost the activity of natural killer cells, which are white blood cells that form your first line of defense by hunting down and disposing of cancer cells. Phytates can also play a role in your last line of defense, which involves starving tumors of their blood supply. There are many phytonutrients in plant foods that can help block the formation of new blood vessels that feed tumors, but phytates also appear able to disrupt existing tumor supply lines. Similarly, many plant compounds appear able to help slow down and even stop cancer cell growth, but phytates can sometimes also cause cancer cells to apparently revert back to their normal state in other words, to stop behaving like cancer. This cancer cell "rehabilitation" has been demonstrated in vitro in colon cancer cells, as well as in cancer cells of the breast, liver, and prostate.
Phytates do have side effects, but they all appear to be good. High phytate intake has been associated with less heart disease, less diabetes, and fewer kidney stones. In fact, some researchers have suggested that phytates be considered an essential nutrient. Like vitamins, phytates participate in important biochemical reactions in the body. Your levels fluctuate with dietary intake, and insufficient consumption is associated with diseases that can be moderated by eating adequate amounts. Maybe phytates should be considered “Vitamin P."
Reversing Rectal Polyps with Berries?
There are many ways the healthfulness of different fruits and vegetables can be compared, such as by nutrient content or antioxidant activity. Ideally, we would use a measure involving actual biological activity. One way to do this is by measuring the suppression of cancer cell growth. Eleven common fruits were tested by dripping their extracts on cancer cells growing in a petri dish. The result? Berries came out on top. Organically grown berries in particular may suppress cancer cell growth better than those grown conventionally. But a laboratory is different from real life. These
findings are only applicable if the active components of the food are absorbed into your system and manage to find their way to budding tumors.
Colorectal cancer, however, grows out of the inner lining of your intestines, so what you eat may have a direct effect regardless. So researchers decided to give berries a try. Familial adenomatous polyposis is an inherited form of colorectal cancer caused by a mutation in your tumor-suppression genes. People who are affected develop hundreds of polyps in their colons, some of which inevitably turn cancerous. Treatment can involve prophylactic colectomy, where the colon is removed early in life as a preventive step. There was a drug that appeared able to cause polyps to regress, but it was pulled from the market after it killed tens of thousands of people. Could berries also cause polyps to retreat without the fatal side effects? Yes. After nine months of daily treatment with black raspberries, the polyp burden of fourteen patients with familial adenomatous polyposis was cut in half. Normally, polyps would have to be surgically removed, but the berries seemed to have made them disappear naturally. The method by which the berries were administered, though, was anything but natural. The researchers used a shortcut, giving the berries as suppositories. After they inserted the equivalent of eight pounds of raspberries into patients' rectums over those nine months, some of the patients suffered from torn anuses. The hope is that research will one day show similar cancer-fighting effects of berries taken the old-fashioned way through the mouth.
Too Much Iron?
In 2012, the results from two major Harvard University studies were published. The first, known as the Nurses Health Study, began following the diets of about 120,000 women aged thirty to fifty-five starting back in 1976; the second, the Health Professionals Follow-Up Study, followed about 50,000 men aged forty to seventy-five. Every four years, researchers checked in with the study participants to keep track of their diets. By 2008, a total of about 24,000 subjects had died, including approximately 6,000 from heart disease and 9,000 from cancer.
After the results were analyzed, the researchers found that the consumption of both processed and unprocessed red meat was associated with an increased risk of dying from cancer and heart disease and shortened life spans overall. They reached this conclusion even after controlling for (factoring in) age, weight, alcohol consumption, exercise, smoking, family history, caloric intake, and even the intake of whole plant foods, such as whole grains, fruits, and vegetables. In other words, the study subjects apparently weren't dying early because they ate less of some beneficial compound like phytates in plants. The findings suggest there may be something harmful in the meat itself. Imagine the logistics of following more than 100,000 people for decades. Now imagine a study five times that size. The largest study of diet and health in history is the NIH-AARP study, cosponsored by the National Institutes of Health and the American Association of Retired Persons. Over the course of a decade, researchers followed about 545,000 men and women aged fifty to seventy-one in the largest study of meat and mortality ever conducted. The scientists came to the same conclusion as the Harvard researchers: Meat consumption was associated with increased risk of dying from cancer, dying from heart disease, and dying prematurely in general. Again, this was after controlling for other diet and lifestyle factors, effectively excluding the possibility that people who ate meat also smoked more, exercised less, or failed to eat their fruits and veggies. The accompanying editorial in the American Medical Association's Archives of Internal Medicine (titled "Reducing Meat Consumption Has Multiple Benefits for the World's Health") called for a major reduction in total meat intake.
What does meat contain that may raise the risk of premature death? One of the possibilities is heme iron, the form of iron found predominantly in blood and muscle. Because iron can generate cancer-causing free radicals by acting as a pro-oxidant, iron can be considered a double-edged sword—too little of it and you risk anemia, too much and you may increase risk of cancer and heart disease. The human body has no specific mechanism to rid itself of excess iron.68
Instead, humans have evolved to tightly regulate the amount of iron absorbed. If you don't have enough iron circulating in your body, your intestines begin boosting iron absorption; if you have too much iron in circulation, your intestines decrease absorption. But this thermostat-like system only works effectively with the primary source of iron in the human diet: the nonheme iron variety found predominantly in plant foods. Once you have a sufficient amount of iron in your blood, your body is about five times more effective at blocking the absorption of excess iron from plant foods than from animal foods.69 This may be why heme iron is associated with cancer70 and heart disease risk. Similarly, heme iron is associated with higher risk of diabetes, but nonheme iron is not.
If we remove iron from people's bodies, can we decrease cancer rates? Studies have found that people randomized to give regular blood donations to reduce their iron stores appear to cut their risk of getting and dying from new gut cancers by about half over a five-year period. The findings were so remarkable that an editorial in the Journal of the National Cancer Institute responded that these results almost seem too good to be true. Donating blood is great, but we should also try to prevent the excess buildup of iron in the first place. The meat industry is working on coming up with additives that suppress the toxic effects of heme iron, but a better strategy may be to emphasize plant sources in your diet, which your body can better manage on a Plant-Based Diet.
Compared with people who eat meat, vegetarians tend to consume more iron (as well as more of most nutrients), but the iron in plant foods is not absorbed as efficiently as the heme iron in meat. While this can be an advantage in preventing iron overload, about one in thirty menstruating women in the United States lose more iron than they take in, which can lead to anemia. Women who eat plant-based diets do not appear to have higher rates of iron deficiency anemia than women who eat a lot of meat, but all women of childbearing age need to ensure adequate iron intake. Those diagnosed with iron deficiency should talk with their doctors about first trying to treat it with diet, as iron supplements have been shown to increase oxidative stress. The healthiest sources of iron are whole grains, legumes, nuts, seeds, dried fruits, and green, leafy vegetables. Avoid drinking tea with meals, as that can inhibit iron absorption. Consuming vitamin C-rich foods can improve iron absorption. The amount of vitamin C in a single orange can enhance iron absorption as much as three to six-fold, so those trying to boost their iron absorption should reach for some fruit instead of a cup of tea.
PANCREATIC CANCER
Pancreatic cancer is among the most lethal forms of cancer, with just 6 percent of patients surviving five years after diagnosis. Thankfully, it's relatively rare, killing only about forty thousand Americans each year. As many as 20 percent of pancreatic cancer cases may be a result of tobacco smoking. Other modifiable risk factors include obesity and heavy alcohol consumption. As we'll see, specific dietary factors may also play a significant role in the development of this deadly disease.
For instance, how the fat in one's diet may contribute to pancreatic cancer risk has long been a subject of debate. The inconsistency of research findings on the impact of total fat intake may be partly because different fats affect risk differently. The previously mentioned NIH-AARP study was large enough to be able to tease out what kind of fat was most associated with pancreatic cancer. It was the first to separate out the role of fats from plant sources, such as those found in nuts, seeds, avocados, and olive and vegetable oils, versus all animal sources, including meats, dairy products, and eggs. The consumption of fat from all animal sources was significantly associated with pancreatic cancer risk, but no correlation was found with the consumption of plant fats.
Chicken and Pancreatic Cancer Risk
Starting in the early 1970s, a series of laws have restricted the use of asbestos, vet thousands of Americans continue to die every year from exposure to it. The Centers for Disease Control and Prevention, the American Academy of Pediatrics, and the Environmental Protection Agency have estimated that over a period of thirty years, approximately one thousand cases of cancer will occur among people exposed to asbestos in school buildings as children. It all started generations ago with the asbestos workers. The first asbestos-related cancers occurred in the 1920s among miners digging up the stuff. Then came a second wave among shipbuilders and construction workers who used asbestos. We are now in the third wave of asbestos-related disease, as buildings constructed with asbestos are beginning to deteriorate.
As the history of asbestos shows, to see if something causes cancer, scientists first study those who have the greatest exposure to it. That's how we're now learning about the potential cancer-causing effects of poultry viruses. There has been long-standing concern about the possibility that wart-causing chicken cancer viruses are being transmitted to the general population through the handling of fresh or frozen chicken. These viruses are known to cause cancer in the birds, but their role in human cancers is unknown. This concern arises out of studies that show that people who work in poultry slaughtering and processing plants have increased risk of dying from certain cancers.
The most recent, a study of thirty thousand poultry workers, was designed specifically to test whether exposure to poultry cancer-causing viruses that widely occurs occupationally in poultry workers not to mention the general population may be associated with increased risks of deaths from liver and pancreatic cancers. The study found that those who slaughter chickens have about nine times the odds of both pancreatic cancer and liver cancer. To put this result in context, the most carefully studied risk factor for pancreatic cancer is cigarette smoking. But even if you smoked for fifty years, you'd have "only" doubled your odds of getting pancreatic cancer.
What about people who eat chicken? The largest study to ever address that question is the European Prospective Investigation into Cancer and Nutrition (EPIC) study, which followed 477,000 people for about a decade. The researchers found a 72 percent increased risk of pancreatic cancer for every fifty grams of chicken consumed daily. And that's not much meat, under two ounces just about a quarter of a chicken breast. The researchers expressed surprise that it was the consumption of poultry not red meat that was more closely tied to cancer. When a similar result was found for lymphomas and leukemias, the same EPIC research team acknowledged that while the growth promoting drugs fed to chickens and turkeys could be playing a role, it might also be cancer viruses found in poultry.
The reason the connection between asbestos and cancer was comparatively easy to nail down is that asbestos caused a particularly unusual cancer (mesothelioma), which was virtually unknown before widespread asbestos use. But because the pancreatic cancer one might get from eating chicken is the same pancreatic cancer one might get from smoking cigarettes, it's more difficult to tease out a cause-and-effect relationship. There are diseases unique to the meat industry, such as the newly described salami brusher's disease that only affects people whose full-time job is to wire-brush off the white mold that naturally grows on salami. But most diseases suffered by meat industry workers are more universal.
Treating Pancreatic Cancer with Curry
Pancreatic cancer is among the most aggressive forms of cancer. Untreated, most patients die two to four months after diagnosis. Unfortunately, only about 10 percent of patients appear to respond to chemotherapy, with the majority suffering severe side effects. Curcumin, the colorful component of the spice turmeric, appears able to reverse precancerous changes in colon cancer and has been shown in laboratory studies to be effective against lung cancer cells. Similar results were obtained using pancreatic cancer cells. So why not try using curcumin to treat patients with pancreatic cancer in a study funded by the National Cancer Institute and performed at the MD Anderson Cancer Center, patients with advanced pancreatic cancer were given large doses of curcumin. Of the twenty-one patients the researchers were able to evaluate, two responded positively to the treatment. One had a 73 percent reduction in his tumor size, though eventually a curcumin-resistant tumor developed in its place.
The other patient, however, showed steady improvement over the course of eighteen months. The only time cancer markers bumped up was during a brief three week period when the curcumin therapy was halted. Yes, the tumors of only two out of twenty-one participants responded, but that's about the same as the chemo regimen, and zero adverse effects were reported with the curcumin treatment. As a result, curcumin is certainly recommended to pancreatic cancer sufferers regardless of what other treatments they choose. Given the tragic prognosis, though, prevention is critical. Until we know more, your best bet is to avoid tobacco, excess alcohol intake, and obesity and to eat a diet low in animal products, refined grains, and added sugars and rich in beans, lentils, split peas, and dried fruit.
ESOPHAGEAL CANCER
Esophageal cancer occurs when cancer cells develop in the esophagus, the muscular tube carrying food from your mouth to your stomach. Typically, the cancer arises in the lining of the esophagus and then invades the outer layers before metastasizing (spreading) to other organs. Early on, there may be few symptoms—if any at all. But as the cancer grows, swallowing difficulties can develop. Every year, there are about eighteen thousand new cases of esophageal cancer and fifteen thousand deaths. The primary risk factors include smoking, heavy alcohol consumption, and gastroesophageal reflux disease (GERD, also called acid reflux), in which acid from the stomach gurgles up into the esophagus, burning the inner layer and causing inflammation that can eventually lead to cancer. Besides avoiding tobacco and alcohol (even light drinking appears to increase risk), the most important thing you can do to prevent esophageal cancer is to eliminate acid reflux disease and that can often be accomplished through diet.
Acid Reflux and Esophageal Cancer
Acid reflux is one of the most common disorders of the digestive tract. The usual symptoms include heartburn as well as the regurgitation of stomach contents back up toward the throat, which can leave a sour taste in the mouth. GERD causes millions of doctor visits and hospitalizations each year and represents the highest annual cost of all digestive diseases in the United States. Chronic inflammation caused by acid reflux can lead to Barrett's esophagus, a precancerous condition that involves changes in the esophageal lining. To prevent adenocarcinoma, the most common type of esophageal cancer in the United States, this sequence of events must be stopped and that means halting acid reflux in the first place. That's a tall order in the United States. Over the past three decades, the incidence of esophageal cancer in Americans has increased six-fold -- an increase greater than that of breast or prostate cancer, and it may be chiefly because acid reflux is on the rise. In the United States, about one in four people (28 percent) suffer at least weekly heartburn and/or acid regurgitation, compared to just 5 percent of the population in Asia.
Over the past two decades, about forty-five studies have examined the link between diet, Barrett's esophagus, and esophageal cancer. The most consistent association with cancer was the consumption of meat and high-fat meals.106 Interestingly, different meats were associated with cancers in different locations. Red meat is strongly associated with cancer in the esophagus itself, whereas poultry was more strongly associated with cancer down around the stomach-
esophagus border. How does this happen? Within five minutes of eating fat, your sphincter muscle at the top of your stomach which acts like a valve to keep down food inside the stomach relaxes, allowing acids to creep back up into the esophagus. For example, in one study, volunteers consuming a high-fat meal (McDonald's sausage, egg, and cheese sandwich) experienced more acid squirting up into their esophagus than those eating a lower-fat meal (McDonald's hotcakes). Part of this effect may be due to the release of a hormone called cholecystokinin, which is triggered by both meat and eggs and may also relax the sphincter. This helps explain why those who eat meat have been found to have twice the odds of reflux-induced esophageal inflammation compared with vegetarians.
Even without the cancer risk, GERD itself can cause pain, bleeding, and scar tissue narrowing of the esophagus that can interfere with swallowing, Billions of dollars are spent on medications to alleviate heartburn and acid reflux by reducing the amount of stomach acid produced, but these drugs can contribute to nutrient deficiencies and increase the risk of pneumonia, intestinal infections, and bone fractures. Perhaps the better strategy would be to just keep the acid in its place by minimizing the intake of foods that allow acid to escape. The protection afforded by plant-based eating may not be based just on the foods that are reduced, though. Centering your diet around antioxidant-rich plant foods may cut in half your odds of esophageal cancer. The most protective foods for cancer at the esophagus-stomach border appear to be red, orange, and dark-green leafy vegetables, berries, apples, and citrus fruits, but all unprocessed plant foods have the advantage of containing fiber.
Fiber and Hiatal Hernia
While fat intake is associated with increased risk of reflux, fiber intake appears to decrease that risk." High fiber intake may reduce the incidence of esophageal cancer by as much as one-thirds by helping to prevent the root cause of many cases of acid reflux: the herniation of part of the stomach up into the chest cavity. Hiatal hernia, as this condition is known, occurs when part of the stomach is pushed up through the diaphragm into the chest. More than one in five Americans suffer from hiatal hernias. In contrast, hiatal hernias are almost unheard of among populations whose diets are plant based, with rates closer to one in a thousand. This is thought to be because they smoothly pass
large, soft stools.
People who don't eat an abundance of whole plant foods have smaller, firmer stools that can be difficult to pass. If you regularly strain to push out stool, over time the increased pressure can push part of the stomach up and out of the abdomen, allowing acid to flow up toward the throat. This same pressure from straining on the toilet week after week can cause other problems. Similar to the way squeezing a stress ball causes a balloon bubble to pop out, the pressure from straining at the toilet may herniate outpouchings from the wall of the colon, a condition known as diverticulosis.
The increased abdominal pressure may also back up blood flow in the veins around the anus, causing hemorrhoids, and even push blood flow back into the legs, resulting in varicose veins. But a fiber-rich diet can relieve the pressure in both directions. Those who eat diets that revolve around whole plant foods tend to pass such effortless bowel movements that their stomachs stay where they're supposed to, which can reduce the acid spillover implicated in one of our deadliest cancers.
Can Strawberries Reverse the Development of Esophageal Cancer?
Esophageal cancer joins pancreatic cancer as one of the gravest diagnoses imaginable. The five-year survival rate is less than 20 percent, with most people dying within the first year after diagnosis. This underscores the need to prevent, stop, or reverse the disease process as early as possible. Researchers decided to put berries to the test. In a randomized clinical trial of powdered strawberries in patients with precancerous lesions in their esophagus, subjects ate one to two ounces of freeze-dried strawberries every day for six months--that's the daily equivalent of about a pound of fresh strawberries.
All of the study participants started out with either mild or moderate precancerous disease, but, amazingly, the progression of the disease was reversed in about 80 percent of the patients in the high-dose strawberry group. Most of these precancerous lesions either regressed from moderate to mild or disappeared entirely. Half of those on the high-dose strawberry treatment walked away disease-free. Fiber consumption doesn't just take off the pressure. Humans evolved eating huge amounts of fiber, likely in excess of one hundred grams daily. That's up to about ten times what the average person eats today. Because plants don't tend to run as fast as animals, the bulk of our diet used to be made up of a lot of bulk. In addition to keeping you regular, fiber binds to toxins, such as lead and mercury, and flushes them away. Our bodies were designed to expect an ever-flowing fiber stream, so it dumps such unwanted waste products as excess cholesterol and estrogen into the intestines, assuming they will be swept away. But if you aren't constantly filling your bowels with plant foods, the only natural source of fiber, unwanted waste products can get reabsorbed and undermine your body's attempts at detoxifying itself. Only 3 percent of Americans may even reach the recommended minimum daily intake of fiber, making it one of the most widespread nutrient deficiencies in the United States at most one drink per day.
Three of the most common cancers of the digestive tract kill approximately one hundred thousand Americans each year. Colorectal (colon and rectal) cancer, which claims fifty thousand lives annually, ranks among the most commonly diagnosed of all cancers. Thankfully, it is also among the most treatable if caught early enough. Pancreatic cancer, on the other hand, is virtually a death sentence for the approximately forty-six thousand people who develop it every year. Few survive beyond a year after diagnosis, which means prevention is paramount. Esophageal cancer, which affects the tube between your mouth and stomach, is also frequently fatal for its eighteen thousand annual victims. The foods you eat can indirectly affect cancer risk, for example, by exacerbating acid reflux, a risk factor for esophageal cancer, or through direct contact with the lining of the digestive tract.
COLORECTAL CANCER
The average person has about a one-in-twenty chance of developing colorectal cancer over the course of his or her lifetime. Fortunately, it is among the most treatable cancers, as regular screening has enabled doctors to detect and remove the cancer before it spreads. There are more than one million colorectal cancer survivors in the United States alone, and, among those diagnosed before the cancer has spread beyond the colon, the five-year survival rate is about 90 percent. But, in its early stages, colorectal cancer rarely causes symptoms. If the cancer is not caught until later stages, treatment is more difficult and less effective. Starting at age fifty until age seventy-five, you should either get stool testing every year, stool testing every three years plus a sigmoidoscopy every five years, or a colonoscopy every ten years. For more on the risks and benefits of these options. While regular screenings are certainly sensible to detect colorectal cancer, preventing it in the first place is even better.
TURMERIC
India's gross domestic product (GDP) is about eight times less than that of the United States," and about 20 percent of its population lives below the poverty line, yet cancer rates in India are much lower than in the United States. Women
in the United States may have ten times more colorectal cancer than women in India, seventeen times more lung cancer, nine times more endometrial cancer and melanoma, twelve times more kidney cancer, eight times more bladder cancer, and five times more breast cancer. Men in the United States appear to have eleven times more colorectal cancer than men in India, twenty-three times more prostate cancer, fourteen times more melanoma, nine times more kidney cancer, and seven times more lung and bladder cancer. Why such a discrepancy? The regular use of the spice turmeric in Indian cooking has been proposed as one possible explanation.
Curcumin, the yellow pigment in the spice turmeric, may be effective against cancer cells in vitro. Very little of the curcumin you eat gets absorbed into your bloodstream, however, so it may never come in sufficient contact with tumors outside the digestive tract. But what doesn't get absorbed into your blood ends up in your colon, where it could impact the cells lining your large intestine where cancerous polyps develop.
The emergence of colorectal cancer can be broken up into three stages. The first sign may be what are called "aberrant crypt foci, or abnormal clusters of cells along the lining of the colon. Next come polyps that grow from that inner surface. The final stage is thought to occur when a benign polyp transforms into a cancerous one. The cancer can then eat through the wall of the colon and spread throughout the body. To what degree can curcumin block each stage
of colorectal cancer?
Studying smokers, who tend to have a lot of aberrant crypt foci, investigators found that curcumin consumption could reduce the number of those cancer-associated structures in their rectums up to nearly 40 percent, from eighteen down to eleven, within just thirty days. The only reported side effect was a yellow tint to their stools. What if polyps have already developed? Six months of curcumin, along with another phytonutrient called quercetin, which is found naturally in such fruits and vegetables as red onions and grapes, were found to decrease the number and size of polyps by more than half in patients with a hereditary form of colorectal cancer. Again, virtually no side effects were reported."
What if the polyps have already transformed into cancer? In a last-ditch attempt to save the lives of fifteen patients with advanced colorectal cancer who didn't respond to any of the standard chemotherapy agents or radiation, oncologists started them on a turmeric extract. In the two to four months of treatment, it appeared to help stall the disease in one-third of the patients, five out of fifteen. If we were talking about some new kind of chemotherapy drug that only helped one in three people, you'd have to weigh that against all the serious side effects. But when it's just some plant extract shown to be remarkably safe, even if it just helped one in a hundred, it would be worth considering.
With no serious downsides, a one-in-three potential benefit for end-stage cancer seems like it would spark further research, right? But who's going to pay for a study of something that can't be patented? The low cancer rate in India may be due in part to the spices they use, but it may also stem from the types of foods they are putting those spices on. India is one of the world's largest producers of fruits and vegetables, and only about 7 percent of the adult population eats meat on a daily basis. What most of the population does eat every day are dark-green, leafy vegetables and legumes, such as beans, split peas, chickpeas, and lentils, which are packed with another class of cancer-fighting compounds called phytates.
STOOL SIZE MATTERS
The bigger and more frequent your bowel movements are, the healthier you may be. Based on a study of twenty-three populations across a dozen countries, the incidence of colon cancer appears to skyrocket as the average daily stool weight drops below about a half a pound. Populations dropping quarter pounders appear to have three times the rate of colon cancer. You can measure the weight of your stools with a simple bathroom scale. No, not that way-by weighing yourself before and after you "go." The link between stool size and colon cancer may be related to "intestinal transit time," the number of hours it takes for food to travel from mouth to toilet. The larger the stool, the quicker the transit time, as it's easier for your intestines to move things along. People don't realize you can have daily bowel movements and still effectively be constipated; what you're flushing today you may have eaten last week. How long it takes food to get from one end to the other can depend on gender and dietary habits. Food goes through men eating plant-based diets in just a day or two, but this transit time takes as long as five or more days among those eating more conventional diets. Women eating plant-based diets also average a day or two, but the average intestinal transit time in most women eating conventional diets may be four days. So you can be regular but four days late.
You can measure your own oral-anal transit time by eating some beets and noting when your stools turn pink. If that takes less than twenty-four to thirty-six hours, you're probably meeting the healthy half pound target. Constipation is the most common gastrointestinal complaint in the United States, leading to millions of doctor visits each year. But beyond just the discomfort, the straining associated with trying to pass small, firm stools may play a role in a host of health problems, including hiatal hernia, varicose veins, hemorrhoids, and painful conditions with names like anal fissure. Constipation can be considered a nutrient-deficiency disease, and that nutrient is fiber. Just as you can get scurvy if you don't get enough vitamin C, you can get constipation if you don't get enough fiber. Since fiber is found only in plant foods, it's no surprise that the more plants you eat, the less likely you are to be constipated. For example, a study comparing thousands of omnivores, vegetarians, and vegans found that those eating strictly plant-based diets are three times more likely to have daily bowel movements. Looks like vegans are just regular people.
PHYTATES
Colorectal cancer is the second-leading cause of cancer-related death in the United States and in some parts of the world, it's practically unheard of. The highest rates have been recorded in Connecticut, and the lowest in Kampala Uganda. Why is colorectal cancer so much more prevalent in Western cultures? Seeking answers to this question, renowned surgeon Denis Burkitt spent twenty-four years in Uganda. Many of the Ugandan hospitals Dr. Burkitt visited had never even seen a case of colon cancer." He eventually came to the conclusion that fiber intake was the key, as most Ugandans consumed diets centered around whole plant foods.
Subsequent research has suggested that dietary prevention of cancer may involve something other than just fiber. For instance, colorectal cancer rates are higher in Denmark than in Finland, yet Danes consume slightly more dietary fiber than Finns. What other protective compounds might explain the low cancer rates among plant-based populations? Well, fiber isn't the only thing found in whole plant foods that's missing from processed and animal-based foods. The answer might lie in natural compounds called phytates, which are found in the seeds of plants in other words, in all whole grains, beans, nuts, and seeds. Phytates have been shown to detoxify excess iron in the body, which otherwise can generate a particularly harmful kind of free radical called hydroxyl radicals. The standard American diet may therefore be a double whammy when it comes to colorectal cancer: Meat contains the type of iron (heme) particularly associated with colorectal cancer but lacks, as do refined plant foods, the phytates to extinguish these iron-forged free radicals.
For many years, phytates were maligned as inhibitors of mineral absorption, which is why you might have heard advice to roast, sprout, or soak your nuts to get rid of the phytates. In theory, this would allow you to absorb more minerals, such as calcium. This belief stemmed from a series of laboratory experiments on puppies from 1949 that suggested that phytates had a bone-softening, anti-calcifying effect, as well as from subsequent studies with similar findings on rats. But more recently, in light of actual human data, phytates image has undergone a complete makeover. Those who eat more high-phytate foods actually tend to have a greater bone mineral density, less bone loss, and fewer hip fractures. Phytates appear to protect bone in a manner similar to that of antiosteoporosis drugs like Fosamax, but without the risk of osteonecrosis (bone rot) of the jaw, a rare, potentially disfiguring side effect associated with that class of drugs.
Colorectal cancer is the second-leading cause of cancer-related death in the United States, and in some parts of the world, it's practically unheard of. The highest rates have been recorded in Connecticut, and the lowest in Kampala Uganda. Why is colorectal cancer so much more prevalent in Western cultures? Seeking answers to this question, renowned surgeon Denis Burkitt spent twenty-four years in Uganda. Many of the Ugandan hospitals Dr. Burkitt visited had never even seen a case of colon cancer. He eventually came to the conclusion that fiber intake was the key, as most Ugandans consumed diets centered around whole plant foods. Subsequent research has suggested that dietary prevention of cancer may involve something other than just fiber. For instance, colorectal cancer rates are higher in Denmark than in Finland, yet Denis consume slightly more dietary fiber than Finns. What other protective compounds might explain the low cancer rates among plant-based populations? Well, fiber isn't the only thing found in whole plant foods that's missing from processed and animal-based foods.
The answer might lie in natural compounds called phytates, which are found in the seeds of plants in other words, in all whole grains, beans, nuts, and seeds. Phytates have been shown to detoxify excess iron in the body, which otherwise can generate a particularly harmful kind of free radical called hydroxyl radicals. The standard American diet may therefore be a double whammy when it comes to colorectal cancer: Meat contains the type of iron (heme) particularly associated with colorectal cancer but lacks, as do refined plant foods, the phytates to extinguish these iron-forged free radicals.
For many years, phytates were maligned as inhibitors of mineral absorption, which is why you might have heard advice to roast, sprout, or soak your nuts to get rid of the phytates. In theory, this would allow you to absorb more minerals, such as calcium. This belief stemmed from a series of laboratory experiments on puppies from 1949 that suggested that phytates had a bone softening, anti calcifying effect, as well as from subsequent studies with similar findings on rats. But more recently, in light of actual human data, those who eat more high-phytate foods actually tend to have a greater bone mineral density, less bone loss, and fewer hip fractures. Phytates appear to protect bone in a manner similar to that of antiosteoporosis drugs like Fosamax, but without the risk of osteonecrosis (bone rot) of the jaw, a rare, potentially disfiguring side effect associated with that class of drugs.
Phytates may also help protect against colorectal cancer. A six-year study of about thirty thousand Californians found that higher meat consumption was associated with higher risk of colon cancer. Unexpectedly, white meat appeared to be worse. Indeed, those who ate red meat at least once each week had about double the risk of developing colon cancer; that risk appeared to triple, however, for those who ate chicken or fish once or more a week. Eating beans, an excellent source of phytates, was found to help mediate some of that risk, so your colon cancer risk may be determined by your meat-to-vegetable ratio. There may be as much as an eightfold difference in colorectal cancer risk between the two extremes-high-vegetable, low-meat diets and low-vegetable, high-meat diets. So it may not be enough to just cut down on how much meat is in your diet; you also need to eat more plants.
The National Cancer Institute's Polyp Prevention Trial found that those who increased their bean consumption by even less than one-quarter cup a day appeared to cut their odds of precancerous colorectal polyp recurrence by up to 65 percent. Of all the wonderful nutrients in beans, why do we credit the phytates with reduced risk? Petri-dish studies have shown that phytates inhibit the growth of virtually all human cancer cells tested so far-including cancers of the colon, breast, cervix, prostate, liver, pancreas, and skin while leaving normal cells alone. This is the mark of a good anticancer agent, the ability to discriminate between tumor cells and normal tissue. When you eat whole grains, beans, nuts, and seeds, phytates are rapidly absorbed into the bloodstream and readily taken up by tumor cells. Tumors concentrate these compounds so efficiently that phytate scans can be used to trace the spread of cancer within the body.
Phytates target cancer cells through a combination of antioxidant, anti-inflammatory, and immune-enhancing activities. Besides affecting the cancer cells directly, phytates have been found to boost the activity of natural killer cells, which are white blood cells that form your first line of defense by hunting down and disposing of cancer cells. Phytates can also play a role in your last line of defense, which involves starving tumors of their blood supply. There are many phytonutrients in plant foods that can help block the formation of new blood vessels that feed tumors, but phytates also appear able to disrupt existing tumor supply lines. Similarly, many plant compounds appear able to help slow down and even stop cancer cell growth, but phytates can sometimes also cause cancer cells to apparently revert back to their normal state in other words, to stop behaving like cancer. This cancer cell "rehabilitation" has been demonstrated in vitro in colon cancer cells, as well as in cancer cells of the breast, liver, and prostate.
Phytates do have side effects, but they all appear to be good. High phytate intake has been associated with less heart disease, less diabetes, and fewer kidney stones. In fact, some researchers have suggested that phytates be considered an essential nutrient. Like vitamins, phytates participate in important biochemical reactions in the body. Your levels fluctuate with dietary intake, and insufficient consumption is associated with diseases that can be moderated by eating adequate amounts. Maybe phytates should be considered “Vitamin P."
Reversing Rectal Polyps with Berries?
There are many ways the healthfulness of different fruits and vegetables can be compared, such as by nutrient content or antioxidant activity. Ideally, we would use a measure involving actual biological activity. One way to do this is by measuring the suppression of cancer cell growth. Eleven common fruits were tested by dripping their extracts on cancer cells growing in a petri dish. The result? Berries came out on top. Organically grown berries in particular may suppress cancer cell growth better than those grown conventionally. But a laboratory is different from real life. These
findings are only applicable if the active components of the food are absorbed into your system and manage to find their way to budding tumors.
Colorectal cancer, however, grows out of the inner lining of your intestines, so what you eat may have a direct effect regardless. So researchers decided to give berries a try. Familial adenomatous polyposis is an inherited form of colorectal cancer caused by a mutation in your tumor-suppression genes. People who are affected develop hundreds of polyps in their colons, some of which inevitably turn cancerous. Treatment can involve prophylactic colectomy, where the colon is removed early in life as a preventive step. There was a drug that appeared able to cause polyps to regress, but it was pulled from the market after it killed tens of thousands of people. Could berries also cause polyps to retreat without the fatal side effects? Yes. After nine months of daily treatment with black raspberries, the polyp burden of fourteen patients with familial adenomatous polyposis was cut in half. Normally, polyps would have to be surgically removed, but the berries seemed to have made them disappear naturally. The method by which the berries were administered, though, was anything but natural. The researchers used a shortcut, giving the berries as suppositories. After they inserted the equivalent of eight pounds of raspberries into patients' rectums over those nine months, some of the patients suffered from torn anuses. The hope is that research will one day show similar cancer-fighting effects of berries taken the old-fashioned way through the mouth.
Too Much Iron?
In 2012, the results from two major Harvard University studies were published. The first, known as the Nurses Health Study, began following the diets of about 120,000 women aged thirty to fifty-five starting back in 1976; the second, the Health Professionals Follow-Up Study, followed about 50,000 men aged forty to seventy-five. Every four years, researchers checked in with the study participants to keep track of their diets. By 2008, a total of about 24,000 subjects had died, including approximately 6,000 from heart disease and 9,000 from cancer.
After the results were analyzed, the researchers found that the consumption of both processed and unprocessed red meat was associated with an increased risk of dying from cancer and heart disease and shortened life spans overall. They reached this conclusion even after controlling for (factoring in) age, weight, alcohol consumption, exercise, smoking, family history, caloric intake, and even the intake of whole plant foods, such as whole grains, fruits, and vegetables. In other words, the study subjects apparently weren't dying early because they ate less of some beneficial compound like phytates in plants. The findings suggest there may be something harmful in the meat itself. Imagine the logistics of following more than 100,000 people for decades. Now imagine a study five times that size. The largest study of diet and health in history is the NIH-AARP study, cosponsored by the National Institutes of Health and the American Association of Retired Persons. Over the course of a decade, researchers followed about 545,000 men and women aged fifty to seventy-one in the largest study of meat and mortality ever conducted. The scientists came to the same conclusion as the Harvard researchers: Meat consumption was associated with increased risk of dying from cancer, dying from heart disease, and dying prematurely in general. Again, this was after controlling for other diet and lifestyle factors, effectively excluding the possibility that people who ate meat also smoked more, exercised less, or failed to eat their fruits and veggies. The accompanying editorial in the American Medical Association's Archives of Internal Medicine (titled "Reducing Meat Consumption Has Multiple Benefits for the World's Health") called for a major reduction in total meat intake.
What does meat contain that may raise the risk of premature death? One of the possibilities is heme iron, the form of iron found predominantly in blood and muscle. Because iron can generate cancer-causing free radicals by acting as a pro-oxidant, iron can be considered a double-edged sword—too little of it and you risk anemia, too much and you may increase risk of cancer and heart disease. The human body has no specific mechanism to rid itself of excess iron.68
Instead, humans have evolved to tightly regulate the amount of iron absorbed. If you don't have enough iron circulating in your body, your intestines begin boosting iron absorption; if you have too much iron in circulation, your intestines decrease absorption. But this thermostat-like system only works effectively with the primary source of iron in the human diet: the nonheme iron variety found predominantly in plant foods. Once you have a sufficient amount of iron in your blood, your body is about five times more effective at blocking the absorption of excess iron from plant foods than from animal foods.69 This may be why heme iron is associated with cancer70 and heart disease risk. Similarly, heme iron is associated with higher risk of diabetes, but nonheme iron is not.
If we remove iron from people's bodies, can we decrease cancer rates? Studies have found that people randomized to give regular blood donations to reduce their iron stores appear to cut their risk of getting and dying from new gut cancers by about half over a five-year period. The findings were so remarkable that an editorial in the Journal of the National Cancer Institute responded that these results almost seem too good to be true. Donating blood is great, but we should also try to prevent the excess buildup of iron in the first place. The meat industry is working on coming up with additives that suppress the toxic effects of heme iron, but a better strategy may be to emphasize plant sources in your diet, which your body can better manage on a Plant-Based Diet.
Compared with people who eat meat, vegetarians tend to consume more iron (as well as more of most nutrients), but the iron in plant foods is not absorbed as efficiently as the heme iron in meat. While this can be an advantage in preventing iron overload, about one in thirty menstruating women in the United States lose more iron than they take in, which can lead to anemia. Women who eat plant-based diets do not appear to have higher rates of iron deficiency anemia than women who eat a lot of meat, but all women of childbearing age need to ensure adequate iron intake. Those diagnosed with iron deficiency should talk with their doctors about first trying to treat it with diet, as iron supplements have been shown to increase oxidative stress. The healthiest sources of iron are whole grains, legumes, nuts, seeds, dried fruits, and green, leafy vegetables. Avoid drinking tea with meals, as that can inhibit iron absorption. Consuming vitamin C-rich foods can improve iron absorption. The amount of vitamin C in a single orange can enhance iron absorption as much as three to six-fold, so those trying to boost their iron absorption should reach for some fruit instead of a cup of tea.
PANCREATIC CANCER
Pancreatic cancer is among the most lethal forms of cancer, with just 6 percent of patients surviving five years after diagnosis. Thankfully, it's relatively rare, killing only about forty thousand Americans each year. As many as 20 percent of pancreatic cancer cases may be a result of tobacco smoking. Other modifiable risk factors include obesity and heavy alcohol consumption. As we'll see, specific dietary factors may also play a significant role in the development of this deadly disease.
For instance, how the fat in one's diet may contribute to pancreatic cancer risk has long been a subject of debate. The inconsistency of research findings on the impact of total fat intake may be partly because different fats affect risk differently. The previously mentioned NIH-AARP study was large enough to be able to tease out what kind of fat was most associated with pancreatic cancer. It was the first to separate out the role of fats from plant sources, such as those found in nuts, seeds, avocados, and olive and vegetable oils, versus all animal sources, including meats, dairy products, and eggs. The consumption of fat from all animal sources was significantly associated with pancreatic cancer risk, but no correlation was found with the consumption of plant fats.
Chicken and Pancreatic Cancer Risk
Starting in the early 1970s, a series of laws have restricted the use of asbestos, vet thousands of Americans continue to die every year from exposure to it. The Centers for Disease Control and Prevention, the American Academy of Pediatrics, and the Environmental Protection Agency have estimated that over a period of thirty years, approximately one thousand cases of cancer will occur among people exposed to asbestos in school buildings as children. It all started generations ago with the asbestos workers. The first asbestos-related cancers occurred in the 1920s among miners digging up the stuff. Then came a second wave among shipbuilders and construction workers who used asbestos. We are now in the third wave of asbestos-related disease, as buildings constructed with asbestos are beginning to deteriorate.
As the history of asbestos shows, to see if something causes cancer, scientists first study those who have the greatest exposure to it. That's how we're now learning about the potential cancer-causing effects of poultry viruses. There has been long-standing concern about the possibility that wart-causing chicken cancer viruses are being transmitted to the general population through the handling of fresh or frozen chicken. These viruses are known to cause cancer in the birds, but their role in human cancers is unknown. This concern arises out of studies that show that people who work in poultry slaughtering and processing plants have increased risk of dying from certain cancers.
The most recent, a study of thirty thousand poultry workers, was designed specifically to test whether exposure to poultry cancer-causing viruses that widely occurs occupationally in poultry workers not to mention the general population may be associated with increased risks of deaths from liver and pancreatic cancers. The study found that those who slaughter chickens have about nine times the odds of both pancreatic cancer and liver cancer. To put this result in context, the most carefully studied risk factor for pancreatic cancer is cigarette smoking. But even if you smoked for fifty years, you'd have "only" doubled your odds of getting pancreatic cancer.
What about people who eat chicken? The largest study to ever address that question is the European Prospective Investigation into Cancer and Nutrition (EPIC) study, which followed 477,000 people for about a decade. The researchers found a 72 percent increased risk of pancreatic cancer for every fifty grams of chicken consumed daily. And that's not much meat, under two ounces just about a quarter of a chicken breast. The researchers expressed surprise that it was the consumption of poultry not red meat that was more closely tied to cancer. When a similar result was found for lymphomas and leukemias, the same EPIC research team acknowledged that while the growth promoting drugs fed to chickens and turkeys could be playing a role, it might also be cancer viruses found in poultry.
The reason the connection between asbestos and cancer was comparatively easy to nail down is that asbestos caused a particularly unusual cancer (mesothelioma), which was virtually unknown before widespread asbestos use. But because the pancreatic cancer one might get from eating chicken is the same pancreatic cancer one might get from smoking cigarettes, it's more difficult to tease out a cause-and-effect relationship. There are diseases unique to the meat industry, such as the newly described salami brusher's disease that only affects people whose full-time job is to wire-brush off the white mold that naturally grows on salami. But most diseases suffered by meat industry workers are more universal.
Treating Pancreatic Cancer with Curry
Pancreatic cancer is among the most aggressive forms of cancer. Untreated, most patients die two to four months after diagnosis. Unfortunately, only about 10 percent of patients appear to respond to chemotherapy, with the majority suffering severe side effects. Curcumin, the colorful component of the spice turmeric, appears able to reverse precancerous changes in colon cancer and has been shown in laboratory studies to be effective against lung cancer cells. Similar results were obtained using pancreatic cancer cells. So why not try using curcumin to treat patients with pancreatic cancer in a study funded by the National Cancer Institute and performed at the MD Anderson Cancer Center, patients with advanced pancreatic cancer were given large doses of curcumin. Of the twenty-one patients the researchers were able to evaluate, two responded positively to the treatment. One had a 73 percent reduction in his tumor size, though eventually a curcumin-resistant tumor developed in its place.
The other patient, however, showed steady improvement over the course of eighteen months. The only time cancer markers bumped up was during a brief three week period when the curcumin therapy was halted. Yes, the tumors of only two out of twenty-one participants responded, but that's about the same as the chemo regimen, and zero adverse effects were reported with the curcumin treatment. As a result, curcumin is certainly recommended to pancreatic cancer sufferers regardless of what other treatments they choose. Given the tragic prognosis, though, prevention is critical. Until we know more, your best bet is to avoid tobacco, excess alcohol intake, and obesity and to eat a diet low in animal products, refined grains, and added sugars and rich in beans, lentils, split peas, and dried fruit.
ESOPHAGEAL CANCER
Esophageal cancer occurs when cancer cells develop in the esophagus, the muscular tube carrying food from your mouth to your stomach. Typically, the cancer arises in the lining of the esophagus and then invades the outer layers before metastasizing (spreading) to other organs. Early on, there may be few symptoms—if any at all. But as the cancer grows, swallowing difficulties can develop. Every year, there are about eighteen thousand new cases of esophageal cancer and fifteen thousand deaths. The primary risk factors include smoking, heavy alcohol consumption, and gastroesophageal reflux disease (GERD, also called acid reflux), in which acid from the stomach gurgles up into the esophagus, burning the inner layer and causing inflammation that can eventually lead to cancer. Besides avoiding tobacco and alcohol (even light drinking appears to increase risk), the most important thing you can do to prevent esophageal cancer is to eliminate acid reflux disease and that can often be accomplished through diet.
Acid Reflux and Esophageal Cancer
Acid reflux is one of the most common disorders of the digestive tract. The usual symptoms include heartburn as well as the regurgitation of stomach contents back up toward the throat, which can leave a sour taste in the mouth. GERD causes millions of doctor visits and hospitalizations each year and represents the highest annual cost of all digestive diseases in the United States. Chronic inflammation caused by acid reflux can lead to Barrett's esophagus, a precancerous condition that involves changes in the esophageal lining. To prevent adenocarcinoma, the most common type of esophageal cancer in the United States, this sequence of events must be stopped and that means halting acid reflux in the first place. That's a tall order in the United States. Over the past three decades, the incidence of esophageal cancer in Americans has increased six-fold -- an increase greater than that of breast or prostate cancer, and it may be chiefly because acid reflux is on the rise. In the United States, about one in four people (28 percent) suffer at least weekly heartburn and/or acid regurgitation, compared to just 5 percent of the population in Asia.
Over the past two decades, about forty-five studies have examined the link between diet, Barrett's esophagus, and esophageal cancer. The most consistent association with cancer was the consumption of meat and high-fat meals.106 Interestingly, different meats were associated with cancers in different locations. Red meat is strongly associated with cancer in the esophagus itself, whereas poultry was more strongly associated with cancer down around the stomach-
esophagus border. How does this happen? Within five minutes of eating fat, your sphincter muscle at the top of your stomach which acts like a valve to keep down food inside the stomach relaxes, allowing acids to creep back up into the esophagus. For example, in one study, volunteers consuming a high-fat meal (McDonald's sausage, egg, and cheese sandwich) experienced more acid squirting up into their esophagus than those eating a lower-fat meal (McDonald's hotcakes). Part of this effect may be due to the release of a hormone called cholecystokinin, which is triggered by both meat and eggs and may also relax the sphincter. This helps explain why those who eat meat have been found to have twice the odds of reflux-induced esophageal inflammation compared with vegetarians.
Even without the cancer risk, GERD itself can cause pain, bleeding, and scar tissue narrowing of the esophagus that can interfere with swallowing, Billions of dollars are spent on medications to alleviate heartburn and acid reflux by reducing the amount of stomach acid produced, but these drugs can contribute to nutrient deficiencies and increase the risk of pneumonia, intestinal infections, and bone fractures. Perhaps the better strategy would be to just keep the acid in its place by minimizing the intake of foods that allow acid to escape. The protection afforded by plant-based eating may not be based just on the foods that are reduced, though. Centering your diet around antioxidant-rich plant foods may cut in half your odds of esophageal cancer. The most protective foods for cancer at the esophagus-stomach border appear to be red, orange, and dark-green leafy vegetables, berries, apples, and citrus fruits, but all unprocessed plant foods have the advantage of containing fiber.
Fiber and Hiatal Hernia
While fat intake is associated with increased risk of reflux, fiber intake appears to decrease that risk." High fiber intake may reduce the incidence of esophageal cancer by as much as one-thirds by helping to prevent the root cause of many cases of acid reflux: the herniation of part of the stomach up into the chest cavity. Hiatal hernia, as this condition is known, occurs when part of the stomach is pushed up through the diaphragm into the chest. More than one in five Americans suffer from hiatal hernias. In contrast, hiatal hernias are almost unheard of among populations whose diets are plant based, with rates closer to one in a thousand. This is thought to be because they smoothly pass
large, soft stools.
People who don't eat an abundance of whole plant foods have smaller, firmer stools that can be difficult to pass. If you regularly strain to push out stool, over time the increased pressure can push part of the stomach up and out of the abdomen, allowing acid to flow up toward the throat. This same pressure from straining on the toilet week after week can cause other problems. Similar to the way squeezing a stress ball causes a balloon bubble to pop out, the pressure from straining at the toilet may herniate outpouchings from the wall of the colon, a condition known as diverticulosis.
The increased abdominal pressure may also back up blood flow in the veins around the anus, causing hemorrhoids, and even push blood flow back into the legs, resulting in varicose veins. But a fiber-rich diet can relieve the pressure in both directions. Those who eat diets that revolve around whole plant foods tend to pass such effortless bowel movements that their stomachs stay where they're supposed to, which can reduce the acid spillover implicated in one of our deadliest cancers.
Can Strawberries Reverse the Development of Esophageal Cancer?
Esophageal cancer joins pancreatic cancer as one of the gravest diagnoses imaginable. The five-year survival rate is less than 20 percent, with most people dying within the first year after diagnosis. This underscores the need to prevent, stop, or reverse the disease process as early as possible. Researchers decided to put berries to the test. In a randomized clinical trial of powdered strawberries in patients with precancerous lesions in their esophagus, subjects ate one to two ounces of freeze-dried strawberries every day for six months--that's the daily equivalent of about a pound of fresh strawberries.
All of the study participants started out with either mild or moderate precancerous disease, but, amazingly, the progression of the disease was reversed in about 80 percent of the patients in the high-dose strawberry group. Most of these precancerous lesions either regressed from moderate to mild or disappeared entirely. Half of those on the high-dose strawberry treatment walked away disease-free. Fiber consumption doesn't just take off the pressure. Humans evolved eating huge amounts of fiber, likely in excess of one hundred grams daily. That's up to about ten times what the average person eats today. Because plants don't tend to run as fast as animals, the bulk of our diet used to be made up of a lot of bulk. In addition to keeping you regular, fiber binds to toxins, such as lead and mercury, and flushes them away. Our bodies were designed to expect an ever-flowing fiber stream, so it dumps such unwanted waste products as excess cholesterol and estrogen into the intestines, assuming they will be swept away. But if you aren't constantly filling your bowels with plant foods, the only natural source of fiber, unwanted waste products can get reabsorbed and undermine your body's attempts at detoxifying itself. Only 3 percent of Americans may even reach the recommended minimum daily intake of fiber, making it one of the most widespread nutrient deficiencies in the United States at most one drink per day.
|
TURMERIC AND COLON CANCER
RESISTANT STARCH AND COLON CANCER
|
TURMERIC AND PANCREATIC CANCER
STOOL pH & COLON CANCER
|
Blood Cancer
Childhood leukemia is one of the few success stories in our war on cancer, with ten-year survival rates as high as 90 percent. Yet it still affects more children than any other cancer and is ten times more likely to be diagnosed in adults, among whom current treatments are much less effective.
What can we do to help prevent blood cancers in the first place? Blood cancers are sometimes referred to as liquid tumors, since the cancer cells often circulate throughout the body rather than get concentrated in a solid mass. These cancers typically begin undetected in the bone marrow, that spongy tissue in the interior of our bones where red blood cells, white blood cells, and platelets are born. When healthy, your red blood cells deliver oxygen throughout your body, your white blood cells fight off infections, and your platelets help your blood to clot. Most blood cancers involve mutations of the white cells.
Blood cancers can be categorized into three types: leukemia, lymphoma, and myeloma. Leukemia (from the Greek roots leukos, or "white," and haima, or "blood") is a disease in which the bone marrow feverishly produces abnormal white blood cells. Unlike normal ones, these imposters aren't able to fight infection. They also impair the ability of your bone marrow to produce normal red and white cells by crowding out healthy ones, creating a diminished healthy blood cell count that can lead to anemia, infection, and, eventually, death.
Lymphoma is a blood cancer of lymphocytes, which are specialized types of white blood cells. Lymphoma cells multiply quickly and can collect in your lymph nodes, small immune organs that are spread throughout the body, including the armpits, neck, and groin. Lymph nodes help to filter your blood. Like leukemia, lymphoma can crowd out healthy cells and impair your ability to fight infections.
You may have heard of non-Hodgkin's lymphoma. Hodgkin's lymphoma can strike Young adults, but it's a rare and usually treatable form of lymphoma. As its name suggests, non-Hodgkin's lymphoma (NHL) includes all the other dozens of types of lymphoma. They're more common and can be harder to treat. and their risk increases with age. The American Cancer Society estimates that there are seventy thousand new cases of non-Hodgkin's lymphoma each year and about nineteen thousand deaths.
Finally, myeloma is a cancer of plasma cells, which are white blood cells that produce antibodies, the proteins that stick to invaders and infected cells to neutralize or tag them for destruction. Cancerous plasma cells can displace healthy cells from your bone marrow and make abnormal antibodies that can clog the kidneys. About 90 percent of myeloma sufferers are discovered with masses of cancer cells growing in multiple bones of their bodies, hence the common term for this condition, multiple myeloma. Each year, twenty-four thousand people are diagnosed with multiple myeloma, and eleven thousand die. Most people with multiple myeloma live for only a few years after diagnosis. Though treatable, multiple myeloma is considered incurable. That's why prevention is key. Fortunately, dietary changes may reduce our risk of all these blood cancers.
FOODS ASSOCIATED WITH DECREASED RISK OF BLOOD CANCERS
After following more than sixty thousand people for more than a dozen years, University of Oxford researchers found that those who consume a plant-based diet are less likely to develop all forms of cancer combined. The greatest protection appeared to be against blood cancers. The incidence of leukemia, lymphoma, and multiple myeloma among those eating vegetarian diets is nearly half that of those eating meat. Why is this greatly reduced risk of blood cancers associated with a more plant-based diet? The British Journal of Cancer concluded, "More research is needed to understand the mechanisms behind this." While they are figuring out the reasons, why not get a head start and try adding more healthy plant foods to your plates today?
Greens and Cancer
The key to cancer prevention and treatment is to keep tumor cells from multiplying out of control while allowing healthy cells to grow normally. Chemotherapy and radiation can do a great job of wiping out cancer cells, but healthy cells can get caught in the crossfire. Some compounds in plants, though, may be more discriminating. For instance, sulforaphane, considered one of the more active components in cruciferous vegetables, kills human leukemia cells in a petri dish while having little impact on the growth of normal cells. As we've discussed, cruciferous vegetables include broccoli, cauliflower, and kale, but there are many others in this family, such as collard greens, watercress, bokchoy, turnips, arugula, radishes (including horseradish), wasabi, and all types of cabbage.
It's intriguing that dripping cabbage compounds on cancer cells affects them in a laboratory, but what really matters is whether people with blood cancers who eat lots of vegetables actually live longer than those who don't. For about eight years, Yale University researchers followed more than five hundred women with non-Hodgkin's lymphoma. Those who started out eating three or more servings of vegetables daily had a 42 percent improved survival rate over those who ate less. Green, leafy vegetables, including salad and cooked greens, and citrus fruits appeared most protective. It's not clear, though, whether the survival benefit arose from helping to keep the cancer at bay or from improving patients' tolerance to the chemotherapy and radiation treatments they were receiving.
The accompanying editorial in the Journal Leukemia & Lymphoma suggested that a "lymphoma diagnosis may be an important 'teachable' moment to improve diet...." I would suggest you not wait until a cancer diagnosis to clean up your diet. The Lowa Women's Health Study, which has followed more than thirty-five thousand women for decades, found that higher broccoli and other cruciferous vegetable intake was associated with lower risk of getting non-Hodgkin's lymphoma in the first place. Likewise, a study at the Mayo Clinic found that those who ate about five or more servings of green, leafy vegetables a week had roughly half the odds of getting lymphoma compared with those who ate less than one serving a week. Some of the plant-based protection might have been due to the antioxidant properties of fruits and vegetables. Higher dietary intake of antioxidants is associated with significantly lower lymphoma risk. Note: dietary intake, not supplementary intake. Antioxidant supplements don't appear to work as much as whole food does. For example, getting lots of vitamin C in your diet is associated with lower lymphoma risk, but taking in even more vitamin C in pill form did not seem to help. The same was found for carotenoid antioxidants like beta-carotene.
Apparently, pills do not have the same cancer-fighting effects as produce. When it comes to certain other cancers, like those of the digestive tract, antioxidant supplements may even make things worse. Combinations of antioxidants like vitamin A, vitamin E, and beta-carotene in pill form were associated with increased risk of death in those who took them. Supplements contain only a select few antioxidants, whereas your body relies on hundreds of them, all working synergistically to create a network to help the body dispose of free radicals. High doses of a single antioxidant may upset this delicate balance and may actually diminish your body's ability to fight cancer. When you buy antioxidant supplements, you may be doling out money to live a shorter life. Save your cash and your health by eating the real thing: food.
Acai Berries and Leukemia
Açai berries gained celebrity status in 2008 when television personality Dr. Mehmet Oz talked about them on The Oprah Winfrey Show. This spawned a frenzy of knockoff supplements, powders, shakes, and other dubious products bearing the acai berry label but not necessarily containing any of the actual berry. Even major corporations have jumped on the acai bandwagon, including Anheuser-Busch with its 180 Blue with Açai Energy drink and Coca-Cola with its Bossa Nova beverage. This is an all-too-common practice in the "superfruit" supplement and beverage market, where less than a quarter of products sold may even contain the ingredients their labels claim.
The benefits of these products are suspect at best, but there is some preliminary research on real acai berries, which can be purchased as unsweetened frozen pulp. The first study published in the medical literature on the effects of acai on human tissue was performed on leukemia cells. Researchers dripped an acai berry extract on leukemia cells taken from a thirty-six-year-old woman. It appeared to trigger self-destruct reactions in up to 86 percent of the cells. Also, sprinkling some freeze-dried acai berries on immune cells called macrophages (from the Greek words makros and phagein, meaning "big eater") in a petri dish appeared to enable the cells to engulf and devour up to 40 percent more microbes than usual.
Though the leukemia study was done using acai extract at the concentration one might expect to find in the bloodstream after eating the berries, no studies have yet been performed on cancer patients themselves (just cancer cells in a test tube), so more testing is needed. Indeed, the only clinical studies on acai berries published so far were two small industry-funded trials that showed modest benefit for osteoarthritis sufferers and some metabolic parameters of overweight subjects. In terms of antioxidant bang for your buck, acai berries get honorable mention, beating out other superstars, such as walnuts, apples, and cranberries.
The bronze for best bargain, though, goes to cloves, the silver to cinnamon, and the gold for most antioxidants per dollar- according to a USDA database of common foods-goes to purple cabbage. Açai berries, however, would probably make a tastier smoothie.
Curcumin and Multiple Myeloma
As noted, multiple myeloma is one of the most dreaded cancers. It is practically incurable even with aggressive medical treatment. As myeloma cells take over the bone marrow, healthy white blood cells continue to decline in number, which increases your susceptibility to infection. Reduced levels of red blood cells can lead to anemia, and reduced platelet counts can lead to serious bleeding. Once diagnosed, most people survive fewer than five years. Multiple myeloma does not occur out of the blue. It appears to be nearly always preceded by a precancerous condition known as monoclonal gammopathy of undetermined significance, or MGUS. When scientists first discovered MGUS, it was aptly named because, at that time, the significance of finding elevated levels of abnormal antibodies in someone's body was unclear. We now know it's a precursor to multiple myeloma, and about 3 percent of Caucasians over age fifty have it, 27 while the rate among African Americans may be double. MGUS causes no symptoms. You won't even know you have it unless your doctor finds it incidentally during routine blood work. The chance of MGUS progressing into myeloma is about 1 percent per year, which means many MGUS-stricken people may die of other causes before they develop myeloma. However, since multiple myeloma is basically a death sentence, scientists have been desperate to find ways to stop MGUS in its tracks.
Given the safety and efficacy of the turmeric spice component curcumin against other types of cancer cells, researchers from the University of Texas collected multiple myeloma cells and put them in a petri dish. Without any intervention, the cancer cells quadrupled within a few days that's how fast this cancer can grow. But when a little curcumin was added to the broth they were bathing in, the myeloma cells' growth was either stunted or stopped altogether. As we've discovered, stopping cancer in a laboratory is one thing. What about in people? In 2009, a pilot study found that half (five out of ten) of the subjects with MGUS who had particularly high abnormal antibody levels responded positively to curcumin supplements. None (zero out of nine) of those given a placebo experienced a similar drop in antibody levels. Buoyed by this success, scientists conducted a randomized, double-blind, placebo-controlled trial and achieved similarly encouraging results in both patients with MGUS and those with "smoldering" multiple myeloma, an early stage of the disease. This result suggests that a simple spice found in the grocery store might have the ability to slow or stop this horrific cancer in a certain percentage of patients, though we won't know more until longer studies are formed to see if these hopeful changes in blood-work biomarkers translate into changes in actual patient outcomes.
ARE ANIMAL VIRUSES INVOLVED IN HUMAN BLOOD CANCERS?
The reason people eating plant-based diets appear to have much lower rates of blood cancers may be due to the foods they're choosing to eat and/or choosing to avoid. To tease out the role different animal products might play in the myriad blood cancers, we would need to conduct a very large study. Enter the aptly named EPIC study, the European Prospective Investigation into Cancer and Nutrition, which did just that. As we saw in chapter 4, researchers recruited more than four hundred thousand men and women across ten countries and followed them for about nine years. If you recall, regular chicken consumption was associated with an increased risk for pancreatic cancer. Similar findings
were found for blood cancers. Of all the animal products studied (including unusual categories, such as offal, or entrails and organs), poultry tended to be associated with the greatest increased risk of non-Hodgkin's lymphoma, all grades of follicular lymphoma, and B-cell lymphomas, such as B-cell chronic lymphatic leukemia (including small lymphocytic leukemia and prolymphocytic lymphocytic leukemia). The EPIC study found that risk increased between 56 percent and 280 percent for every 50 grams of poultry consumed daily. For comparison, a cooked, boneless chicken breast may weigh as much as 384 grams.
Why is there so much lymphoma and leukemia risk associated with eating such relatively small amounts of poultry? The researchers suggested this result could be a fluke, or it could be due to the drugs, such as antibiotics, often fed to chickens and turkeys to promote their growth. Or it might be the dioxins found in some poultry meat, which have been linked to lymphoma.
But dairy can also contain dioxins, and milk consumption was not linked to Non Hodgkins Lymphoma (NHL). The researchers surmised it may be the cancer-causing viruses in poultry, given that lower risk of NHL has been associated with eating meat cooked well done instead of rare (thereby inactivating any viruses). This suggestion is consistent with the results of the NIH-AARP study, which found an association between eating just done chicken and one type of lymphoma and lower risk of another blood cancer tied to greater exposure to the cooked meat carcinogen MelQx.
How could less cancer be linked to more carcinogen exposure? MelQx is one of the heterocyclic amines created by cooking meat at high temperatures, such as baking, broiling, and frying." If, in the case of blood cancers, one cause is a poultry virus, then the more the meat was cooked, the more likely it is that the virus was destroyed. Cancer-causing poultry viruses-including the avian herpesvirus that causes Marek's disease, several retroviruses like reticuloendotheliosis virus, the avian leukosis virus found in chickens, and the lymphoproliferative disease virus found in turkeys-may explain the higher rates of blood cancers among farmers, 40 slaughterhouse workers, and butchers. Viruses can cause cancer by directly inserting a cancer-causing gene into a host's DNA.
Animal viruses can infect people who prepare meat with unpleasant skin diseases, such as contagious pustular dermatitis.44 There's even a well-defined medical condition commonly known as "butchers' warts" that affects the hands of those who handle fresh meat, including poultry and fish. Even the wives of butchers appear to be at higher risk for cervical cancer, a cancer definitively associated with wart-virus exposure. Workers in poultry slaughterhouses have been found to have higher rates of cancers of the mouth, nasal cavities, throat, esophagus, rectum, liver, and blood. On a public health level, the concern here is that the cancer-causing viruses present in poultry and poultry products may then be transmitted to those in the general population who handle or eat inadequately cooked chicken. These results were replicated recently in the largest such investigation to date, studying more than twenty thousand workers in poultry slaughtering and processing plants. They confirmed the findings of three other studies to date: Workers in these facilities do have increased risk of dying from certain cancers, including cancers of the blood.
Researchers are finally starting to connect the dots. The high levels of antibodies to avian leukosis/sarcoma viruses and to reticuloendotheliosis viruses recently found in poultry workers provide evidence of human exposure to these cancer-causing poultry viruses. Even line workers who simply cut up the finished product and weren't ever exposed to live birds had elevated levels of antibodies in their blood." Beyond just occupational safety, the potential threat to the public, the researchers concluded, "is not trivial." Elevated blood cancer rates can even be traced back to the farm.
An analysis of more than one hundred thousand death certificates found that those who grew up on a farm raising animals appeared significantly more likely to develop a blood cancer later in life, whereas growing up on a farm growing only crops was not. Worst was growing up on a poultry farm, which was associated with nearly three times the odds of developing blood cancer. Exposure to cattle and pigs has also been associated with non-Hodgkin's lymphoma. A 2003 study by University of California researchers revealed that nearly three-quarters of human subjects tested positive for exposure to the bovine leukemia virus, likely through the consumption of meat and dairy products.
Approximately 85 percent of U.S. dairy herds have tested positive for the virus (and 100 percent on industrial-scale operations). However, just because people are exposed to a virus that causes cancer in cows does not mean that humans themselves can become actively infected with it. In 2014, researchers supported in part by the U.S. Army Breast Cancer Research Program published a remarkable report in a journal of the Centers for Disease Control and Prevention. They reported that the bovine leukemia virus DNA was found to be incorporated into normal and cancerous human breast tissue, effectively proving that people can also become infected with this cancer-causing animal virus. To date, however, the role poultry and other farm animal viruses play in the development of human cancers remains unknown.
What about the feline leukemia virus? Thankfully, pet companionship is associated with lower rates of lymphoma, which is a personal relief given how many animals I've shared my life with. And the longer people have had cats or dogs in their lives, the lower their risk. In one study, the lowest risk of lymphoma was found in people who had had pets for twenty years or longer. The researchers suspect the reason is connected to the fact that having pets may have beneficial effects on the immune system. A pair of Harvard University studies suggested that diet soda consumption may increase the risk of non-Hodgkin's lymphoma and multiple myeloma, but this association was only seen among men and was not confirmed in two other large studies on aspartame-sweetened soda.60,61 Eliminating soda can't hurt, though, in addition to making the dietary changes outlined above.
Plant-based diets are associated with nearly half the risk of blood cancers, protection likely to derive both from the avoidance of foods tied to liquid tumors, such as poultry, as well as the additional consumption of fruits and vegetables. Greens may be particularly useful for non-Hodgkin's lymphoma and turmeric for multiple myeloma. The role tumor-promoting farm animal viruses play in human cancers is not known, but this should be a research priority given the potential extent of public exposure.
What can we do to help prevent blood cancers in the first place? Blood cancers are sometimes referred to as liquid tumors, since the cancer cells often circulate throughout the body rather than get concentrated in a solid mass. These cancers typically begin undetected in the bone marrow, that spongy tissue in the interior of our bones where red blood cells, white blood cells, and platelets are born. When healthy, your red blood cells deliver oxygen throughout your body, your white blood cells fight off infections, and your platelets help your blood to clot. Most blood cancers involve mutations of the white cells.
Blood cancers can be categorized into three types: leukemia, lymphoma, and myeloma. Leukemia (from the Greek roots leukos, or "white," and haima, or "blood") is a disease in which the bone marrow feverishly produces abnormal white blood cells. Unlike normal ones, these imposters aren't able to fight infection. They also impair the ability of your bone marrow to produce normal red and white cells by crowding out healthy ones, creating a diminished healthy blood cell count that can lead to anemia, infection, and, eventually, death.
Lymphoma is a blood cancer of lymphocytes, which are specialized types of white blood cells. Lymphoma cells multiply quickly and can collect in your lymph nodes, small immune organs that are spread throughout the body, including the armpits, neck, and groin. Lymph nodes help to filter your blood. Like leukemia, lymphoma can crowd out healthy cells and impair your ability to fight infections.
You may have heard of non-Hodgkin's lymphoma. Hodgkin's lymphoma can strike Young adults, but it's a rare and usually treatable form of lymphoma. As its name suggests, non-Hodgkin's lymphoma (NHL) includes all the other dozens of types of lymphoma. They're more common and can be harder to treat. and their risk increases with age. The American Cancer Society estimates that there are seventy thousand new cases of non-Hodgkin's lymphoma each year and about nineteen thousand deaths.
Finally, myeloma is a cancer of plasma cells, which are white blood cells that produce antibodies, the proteins that stick to invaders and infected cells to neutralize or tag them for destruction. Cancerous plasma cells can displace healthy cells from your bone marrow and make abnormal antibodies that can clog the kidneys. About 90 percent of myeloma sufferers are discovered with masses of cancer cells growing in multiple bones of their bodies, hence the common term for this condition, multiple myeloma. Each year, twenty-four thousand people are diagnosed with multiple myeloma, and eleven thousand die. Most people with multiple myeloma live for only a few years after diagnosis. Though treatable, multiple myeloma is considered incurable. That's why prevention is key. Fortunately, dietary changes may reduce our risk of all these blood cancers.
FOODS ASSOCIATED WITH DECREASED RISK OF BLOOD CANCERS
After following more than sixty thousand people for more than a dozen years, University of Oxford researchers found that those who consume a plant-based diet are less likely to develop all forms of cancer combined. The greatest protection appeared to be against blood cancers. The incidence of leukemia, lymphoma, and multiple myeloma among those eating vegetarian diets is nearly half that of those eating meat. Why is this greatly reduced risk of blood cancers associated with a more plant-based diet? The British Journal of Cancer concluded, "More research is needed to understand the mechanisms behind this." While they are figuring out the reasons, why not get a head start and try adding more healthy plant foods to your plates today?
Greens and Cancer
The key to cancer prevention and treatment is to keep tumor cells from multiplying out of control while allowing healthy cells to grow normally. Chemotherapy and radiation can do a great job of wiping out cancer cells, but healthy cells can get caught in the crossfire. Some compounds in plants, though, may be more discriminating. For instance, sulforaphane, considered one of the more active components in cruciferous vegetables, kills human leukemia cells in a petri dish while having little impact on the growth of normal cells. As we've discussed, cruciferous vegetables include broccoli, cauliflower, and kale, but there are many others in this family, such as collard greens, watercress, bokchoy, turnips, arugula, radishes (including horseradish), wasabi, and all types of cabbage.
It's intriguing that dripping cabbage compounds on cancer cells affects them in a laboratory, but what really matters is whether people with blood cancers who eat lots of vegetables actually live longer than those who don't. For about eight years, Yale University researchers followed more than five hundred women with non-Hodgkin's lymphoma. Those who started out eating three or more servings of vegetables daily had a 42 percent improved survival rate over those who ate less. Green, leafy vegetables, including salad and cooked greens, and citrus fruits appeared most protective. It's not clear, though, whether the survival benefit arose from helping to keep the cancer at bay or from improving patients' tolerance to the chemotherapy and radiation treatments they were receiving.
The accompanying editorial in the Journal Leukemia & Lymphoma suggested that a "lymphoma diagnosis may be an important 'teachable' moment to improve diet...." I would suggest you not wait until a cancer diagnosis to clean up your diet. The Lowa Women's Health Study, which has followed more than thirty-five thousand women for decades, found that higher broccoli and other cruciferous vegetable intake was associated with lower risk of getting non-Hodgkin's lymphoma in the first place. Likewise, a study at the Mayo Clinic found that those who ate about five or more servings of green, leafy vegetables a week had roughly half the odds of getting lymphoma compared with those who ate less than one serving a week. Some of the plant-based protection might have been due to the antioxidant properties of fruits and vegetables. Higher dietary intake of antioxidants is associated with significantly lower lymphoma risk. Note: dietary intake, not supplementary intake. Antioxidant supplements don't appear to work as much as whole food does. For example, getting lots of vitamin C in your diet is associated with lower lymphoma risk, but taking in even more vitamin C in pill form did not seem to help. The same was found for carotenoid antioxidants like beta-carotene.
Apparently, pills do not have the same cancer-fighting effects as produce. When it comes to certain other cancers, like those of the digestive tract, antioxidant supplements may even make things worse. Combinations of antioxidants like vitamin A, vitamin E, and beta-carotene in pill form were associated with increased risk of death in those who took them. Supplements contain only a select few antioxidants, whereas your body relies on hundreds of them, all working synergistically to create a network to help the body dispose of free radicals. High doses of a single antioxidant may upset this delicate balance and may actually diminish your body's ability to fight cancer. When you buy antioxidant supplements, you may be doling out money to live a shorter life. Save your cash and your health by eating the real thing: food.
Acai Berries and Leukemia
Açai berries gained celebrity status in 2008 when television personality Dr. Mehmet Oz talked about them on The Oprah Winfrey Show. This spawned a frenzy of knockoff supplements, powders, shakes, and other dubious products bearing the acai berry label but not necessarily containing any of the actual berry. Even major corporations have jumped on the acai bandwagon, including Anheuser-Busch with its 180 Blue with Açai Energy drink and Coca-Cola with its Bossa Nova beverage. This is an all-too-common practice in the "superfruit" supplement and beverage market, where less than a quarter of products sold may even contain the ingredients their labels claim.
The benefits of these products are suspect at best, but there is some preliminary research on real acai berries, which can be purchased as unsweetened frozen pulp. The first study published in the medical literature on the effects of acai on human tissue was performed on leukemia cells. Researchers dripped an acai berry extract on leukemia cells taken from a thirty-six-year-old woman. It appeared to trigger self-destruct reactions in up to 86 percent of the cells. Also, sprinkling some freeze-dried acai berries on immune cells called macrophages (from the Greek words makros and phagein, meaning "big eater") in a petri dish appeared to enable the cells to engulf and devour up to 40 percent more microbes than usual.
Though the leukemia study was done using acai extract at the concentration one might expect to find in the bloodstream after eating the berries, no studies have yet been performed on cancer patients themselves (just cancer cells in a test tube), so more testing is needed. Indeed, the only clinical studies on acai berries published so far were two small industry-funded trials that showed modest benefit for osteoarthritis sufferers and some metabolic parameters of overweight subjects. In terms of antioxidant bang for your buck, acai berries get honorable mention, beating out other superstars, such as walnuts, apples, and cranberries.
The bronze for best bargain, though, goes to cloves, the silver to cinnamon, and the gold for most antioxidants per dollar- according to a USDA database of common foods-goes to purple cabbage. Açai berries, however, would probably make a tastier smoothie.
Curcumin and Multiple Myeloma
As noted, multiple myeloma is one of the most dreaded cancers. It is practically incurable even with aggressive medical treatment. As myeloma cells take over the bone marrow, healthy white blood cells continue to decline in number, which increases your susceptibility to infection. Reduced levels of red blood cells can lead to anemia, and reduced platelet counts can lead to serious bleeding. Once diagnosed, most people survive fewer than five years. Multiple myeloma does not occur out of the blue. It appears to be nearly always preceded by a precancerous condition known as monoclonal gammopathy of undetermined significance, or MGUS. When scientists first discovered MGUS, it was aptly named because, at that time, the significance of finding elevated levels of abnormal antibodies in someone's body was unclear. We now know it's a precursor to multiple myeloma, and about 3 percent of Caucasians over age fifty have it, 27 while the rate among African Americans may be double. MGUS causes no symptoms. You won't even know you have it unless your doctor finds it incidentally during routine blood work. The chance of MGUS progressing into myeloma is about 1 percent per year, which means many MGUS-stricken people may die of other causes before they develop myeloma. However, since multiple myeloma is basically a death sentence, scientists have been desperate to find ways to stop MGUS in its tracks.
Given the safety and efficacy of the turmeric spice component curcumin against other types of cancer cells, researchers from the University of Texas collected multiple myeloma cells and put them in a petri dish. Without any intervention, the cancer cells quadrupled within a few days that's how fast this cancer can grow. But when a little curcumin was added to the broth they were bathing in, the myeloma cells' growth was either stunted or stopped altogether. As we've discovered, stopping cancer in a laboratory is one thing. What about in people? In 2009, a pilot study found that half (five out of ten) of the subjects with MGUS who had particularly high abnormal antibody levels responded positively to curcumin supplements. None (zero out of nine) of those given a placebo experienced a similar drop in antibody levels. Buoyed by this success, scientists conducted a randomized, double-blind, placebo-controlled trial and achieved similarly encouraging results in both patients with MGUS and those with "smoldering" multiple myeloma, an early stage of the disease. This result suggests that a simple spice found in the grocery store might have the ability to slow or stop this horrific cancer in a certain percentage of patients, though we won't know more until longer studies are formed to see if these hopeful changes in blood-work biomarkers translate into changes in actual patient outcomes.
ARE ANIMAL VIRUSES INVOLVED IN HUMAN BLOOD CANCERS?
The reason people eating plant-based diets appear to have much lower rates of blood cancers may be due to the foods they're choosing to eat and/or choosing to avoid. To tease out the role different animal products might play in the myriad blood cancers, we would need to conduct a very large study. Enter the aptly named EPIC study, the European Prospective Investigation into Cancer and Nutrition, which did just that. As we saw in chapter 4, researchers recruited more than four hundred thousand men and women across ten countries and followed them for about nine years. If you recall, regular chicken consumption was associated with an increased risk for pancreatic cancer. Similar findings
were found for blood cancers. Of all the animal products studied (including unusual categories, such as offal, or entrails and organs), poultry tended to be associated with the greatest increased risk of non-Hodgkin's lymphoma, all grades of follicular lymphoma, and B-cell lymphomas, such as B-cell chronic lymphatic leukemia (including small lymphocytic leukemia and prolymphocytic lymphocytic leukemia). The EPIC study found that risk increased between 56 percent and 280 percent for every 50 grams of poultry consumed daily. For comparison, a cooked, boneless chicken breast may weigh as much as 384 grams.
Why is there so much lymphoma and leukemia risk associated with eating such relatively small amounts of poultry? The researchers suggested this result could be a fluke, or it could be due to the drugs, such as antibiotics, often fed to chickens and turkeys to promote their growth. Or it might be the dioxins found in some poultry meat, which have been linked to lymphoma.
But dairy can also contain dioxins, and milk consumption was not linked to Non Hodgkins Lymphoma (NHL). The researchers surmised it may be the cancer-causing viruses in poultry, given that lower risk of NHL has been associated with eating meat cooked well done instead of rare (thereby inactivating any viruses). This suggestion is consistent with the results of the NIH-AARP study, which found an association between eating just done chicken and one type of lymphoma and lower risk of another blood cancer tied to greater exposure to the cooked meat carcinogen MelQx.
How could less cancer be linked to more carcinogen exposure? MelQx is one of the heterocyclic amines created by cooking meat at high temperatures, such as baking, broiling, and frying." If, in the case of blood cancers, one cause is a poultry virus, then the more the meat was cooked, the more likely it is that the virus was destroyed. Cancer-causing poultry viruses-including the avian herpesvirus that causes Marek's disease, several retroviruses like reticuloendotheliosis virus, the avian leukosis virus found in chickens, and the lymphoproliferative disease virus found in turkeys-may explain the higher rates of blood cancers among farmers, 40 slaughterhouse workers, and butchers. Viruses can cause cancer by directly inserting a cancer-causing gene into a host's DNA.
Animal viruses can infect people who prepare meat with unpleasant skin diseases, such as contagious pustular dermatitis.44 There's even a well-defined medical condition commonly known as "butchers' warts" that affects the hands of those who handle fresh meat, including poultry and fish. Even the wives of butchers appear to be at higher risk for cervical cancer, a cancer definitively associated with wart-virus exposure. Workers in poultry slaughterhouses have been found to have higher rates of cancers of the mouth, nasal cavities, throat, esophagus, rectum, liver, and blood. On a public health level, the concern here is that the cancer-causing viruses present in poultry and poultry products may then be transmitted to those in the general population who handle or eat inadequately cooked chicken. These results were replicated recently in the largest such investigation to date, studying more than twenty thousand workers in poultry slaughtering and processing plants. They confirmed the findings of three other studies to date: Workers in these facilities do have increased risk of dying from certain cancers, including cancers of the blood.
Researchers are finally starting to connect the dots. The high levels of antibodies to avian leukosis/sarcoma viruses and to reticuloendotheliosis viruses recently found in poultry workers provide evidence of human exposure to these cancer-causing poultry viruses. Even line workers who simply cut up the finished product and weren't ever exposed to live birds had elevated levels of antibodies in their blood." Beyond just occupational safety, the potential threat to the public, the researchers concluded, "is not trivial." Elevated blood cancer rates can even be traced back to the farm.
An analysis of more than one hundred thousand death certificates found that those who grew up on a farm raising animals appeared significantly more likely to develop a blood cancer later in life, whereas growing up on a farm growing only crops was not. Worst was growing up on a poultry farm, which was associated with nearly three times the odds of developing blood cancer. Exposure to cattle and pigs has also been associated with non-Hodgkin's lymphoma. A 2003 study by University of California researchers revealed that nearly three-quarters of human subjects tested positive for exposure to the bovine leukemia virus, likely through the consumption of meat and dairy products.
Approximately 85 percent of U.S. dairy herds have tested positive for the virus (and 100 percent on industrial-scale operations). However, just because people are exposed to a virus that causes cancer in cows does not mean that humans themselves can become actively infected with it. In 2014, researchers supported in part by the U.S. Army Breast Cancer Research Program published a remarkable report in a journal of the Centers for Disease Control and Prevention. They reported that the bovine leukemia virus DNA was found to be incorporated into normal and cancerous human breast tissue, effectively proving that people can also become infected with this cancer-causing animal virus. To date, however, the role poultry and other farm animal viruses play in the development of human cancers remains unknown.
What about the feline leukemia virus? Thankfully, pet companionship is associated with lower rates of lymphoma, which is a personal relief given how many animals I've shared my life with. And the longer people have had cats or dogs in their lives, the lower their risk. In one study, the lowest risk of lymphoma was found in people who had had pets for twenty years or longer. The researchers suspect the reason is connected to the fact that having pets may have beneficial effects on the immune system. A pair of Harvard University studies suggested that diet soda consumption may increase the risk of non-Hodgkin's lymphoma and multiple myeloma, but this association was only seen among men and was not confirmed in two other large studies on aspartame-sweetened soda.60,61 Eliminating soda can't hurt, though, in addition to making the dietary changes outlined above.
Plant-based diets are associated with nearly half the risk of blood cancers, protection likely to derive both from the avoidance of foods tied to liquid tumors, such as poultry, as well as the additional consumption of fruits and vegetables. Greens may be particularly useful for non-Hodgkin's lymphoma and turmeric for multiple myeloma. The role tumor-promoting farm animal viruses play in human cancers is not known, but this should be a research priority given the potential extent of public exposure.
Article Review
|
|
|
Unit Task
This unit is essential in understanding the role of diet in cancer prevention and management. In this task you are required to create a REFLECTIVE JOURNAL highlighting the learnings you had from the subsections provided in this unit. At the last portion of your paper, make a self assessment and conduct a thorough review on your own lifestyle and eating behavior to assess if you are getting yourself near the hook of Cancer development. (4-page review - not less than 2000 words)