Nutrition Assessment and Prescription - Unit 1 |
OBJECTIVES:
- Analyze the importance and limitation of global food-based dietary guidelines
- Assess food intake patterns and nutrients of deficit and excess
- Describe the health and environmental impact of adapting Standard American Diet in the developing countries
- Discuss the basic principles in meal planning
- Understand the importance of calorie balance and macronutrient amount in creating a meal plan
Nutrition in Clinical Medicine
In 1957, a surgeon named Denis Burkitt first encountered a puzzling form of childhood cancer. The condition, which came to be called Burkitt's lymphoma, caused a massive swelling of the jaw and was often fatal. But Burkitt noticed something peculiar: The disease followed a geographic pattern, never appearing far from the equator and the east coast of Africa. He painstakingly identified the cause - a virus (known as Epstein-Barr) transmitted by an insect vector - and then found an effective treatment. His lifesaving work was acclaimed throughout the world of medicine.
Soon thereafter, Dr. Burkitt set his sights on larger medical epidemics whose solutions were hidden in much bigger geographical puzzle. He noticed that the great bulk of diseases occurring in the Western world - heart disease, diabetes, obesity, and many others - were surprisingly rare in rural Africa. During 20 years of surgical practice in Africa, he removed only 2 gallbladders, something he might have done on a single morning in London hospital. Many other conditions, from appendicitis to colon cancer, were rare in Africa, but common in Europe. He ruled out genetics as the main explanation, because people moving from one country to another eventually assumed the same risks as the populations in their adopted homes.
Burkitt proposed that the culprit was diet. In Europe and the Americas, diets bore no resemblance to a fiber-rich African diet. On the contrary, they were fiber-depleted and laden with fat, cholesterol, and sugar. His work, and that of other medical pioneers, launched a major rethinking of the fundamental causes of illness. Previously, nutrition had been thought to play a fairly minor role in health. There were rare deficiency states such as pellarga or scurvy, but these were little more than details on medical school examinations. The major killer diseases were thought to have more to do with genes and bad luck than diet. but this new breed of researchers held that nutrition was decisive. It was a fundamental contributor to the major diseases that filled doctors' waiting rooms throughout the Western world.
Soon thereafter, Dr. Burkitt set his sights on larger medical epidemics whose solutions were hidden in much bigger geographical puzzle. He noticed that the great bulk of diseases occurring in the Western world - heart disease, diabetes, obesity, and many others - were surprisingly rare in rural Africa. During 20 years of surgical practice in Africa, he removed only 2 gallbladders, something he might have done on a single morning in London hospital. Many other conditions, from appendicitis to colon cancer, were rare in Africa, but common in Europe. He ruled out genetics as the main explanation, because people moving from one country to another eventually assumed the same risks as the populations in their adopted homes.
Burkitt proposed that the culprit was diet. In Europe and the Americas, diets bore no resemblance to a fiber-rich African diet. On the contrary, they were fiber-depleted and laden with fat, cholesterol, and sugar. His work, and that of other medical pioneers, launched a major rethinking of the fundamental causes of illness. Previously, nutrition had been thought to play a fairly minor role in health. There were rare deficiency states such as pellarga or scurvy, but these were little more than details on medical school examinations. The major killer diseases were thought to have more to do with genes and bad luck than diet. but this new breed of researchers held that nutrition was decisive. It was a fundamental contributor to the major diseases that filled doctors' waiting rooms throughout the Western world.
|
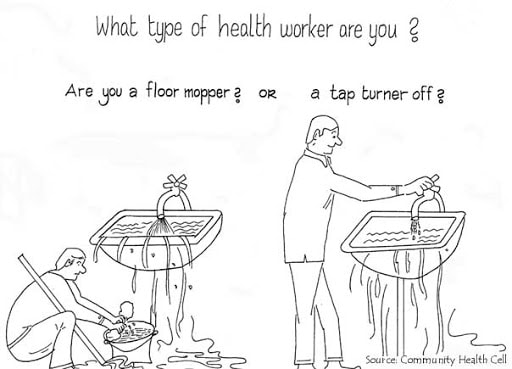
Burkitt proposed that health authorities should spend less time dealing with the results of bad diet and more time encouraging people to change the way they eat.
To continue to treat illnesses while ignoring prevention, he said, was like a plumber mopping up a kitchen floor rather than turning off the faucet in an overflowing sink. A new focus on nutrition and prevention could turn the tide in the epidemics of our time. |
Evolving knowledge in Nutrition
Just as new medications often have advantages over previous ones, diet approaches evolve as well, with new dietary methods building on previous ones and research studies putting diets to the test. Heart-healthy diets are a case in point. For decades, cardiologists have encouraged heart patients to switch from red meat to white meat, trim away chicken skin, and stay physically active. These steps were modestly helpful. Following such guidance, an average patient experienced roughly a 5% drop in low density lipoprotein (LDL) cholesterol.
However, in 1990, a Harvard-trained physician named Dean Ornish published the results of a study using a much more vigorous regimen. His research participants had significant heart disease. His experimental treatment included low-fat, vegetarian diet, smoking cessation, modest exercise, and stress management. The diet was logical: Foods from plants have no cholesterol and no animal fat. For comparison study included a control group that received the usual care that doctors provide for heart patients.
The result made medical history. Not only did the program reduce cholesterol far more effectively than previous diets, it visibly changed the disease process itself. Angiograms done before and after the one-year intervention showed that participants in the control group gradually worsened. But the patients in the experimental group had a very different experience. Their coronary arteries were beginning to open up again, so much so that signs of reversal were clearly evident in 82% of participants within the first year.
In 1999, Dr. Caldwell Esselstyn, a Cleveland Clinic surgeon, published the results of remarkable 12-year study integrating nutrition with medications. In a group of patients with severe heart disease, he used a diet similar to that used by Dr. Ornish. For any patient whose total cholesterol remained above 150 mg/dl despite the diet, he added cholesterol-lowering medications. In the ensuing 12 years, the research participants had no cardiac events. The combination of the the diet and judiciously used medications made the patients practically health-attack-proof.
Then, in 2005, David Jenkins, from the University of Toronto, took things a step further. He emphasized foods with known cholesterol-lowering properties - oats, soy, and certain nuts, for example. In four weeks' time, LDL cholesterol fell nearly 30%. As research has moved forward, our idea of an effective diet has advanced as well.
The same sort of trend has occurred in the approach to cancer. For many years, lifestyle advice from cancer authorities was limited to avoiding tobacco and getting regular checkups. But it has become clear that diet plays a major role in cancer risk. We now encourage all patients to include more fruits and vegetables in their routines, to focus on foods that are rich in antioxidants, and to limit fat and boost fiber.
More recently, nutritional steps have been tested not only for cancer prevention, but for cancer survival. Studies of individuals diagnosed with breast or prostate cancer have shown that diet may make a major difference in the ensuing years.
However, in 1990, a Harvard-trained physician named Dean Ornish published the results of a study using a much more vigorous regimen. His research participants had significant heart disease. His experimental treatment included low-fat, vegetarian diet, smoking cessation, modest exercise, and stress management. The diet was logical: Foods from plants have no cholesterol and no animal fat. For comparison study included a control group that received the usual care that doctors provide for heart patients.
The result made medical history. Not only did the program reduce cholesterol far more effectively than previous diets, it visibly changed the disease process itself. Angiograms done before and after the one-year intervention showed that participants in the control group gradually worsened. But the patients in the experimental group had a very different experience. Their coronary arteries were beginning to open up again, so much so that signs of reversal were clearly evident in 82% of participants within the first year.
In 1999, Dr. Caldwell Esselstyn, a Cleveland Clinic surgeon, published the results of remarkable 12-year study integrating nutrition with medications. In a group of patients with severe heart disease, he used a diet similar to that used by Dr. Ornish. For any patient whose total cholesterol remained above 150 mg/dl despite the diet, he added cholesterol-lowering medications. In the ensuing 12 years, the research participants had no cardiac events. The combination of the the diet and judiciously used medications made the patients practically health-attack-proof.
Then, in 2005, David Jenkins, from the University of Toronto, took things a step further. He emphasized foods with known cholesterol-lowering properties - oats, soy, and certain nuts, for example. In four weeks' time, LDL cholesterol fell nearly 30%. As research has moved forward, our idea of an effective diet has advanced as well.
The same sort of trend has occurred in the approach to cancer. For many years, lifestyle advice from cancer authorities was limited to avoiding tobacco and getting regular checkups. But it has become clear that diet plays a major role in cancer risk. We now encourage all patients to include more fruits and vegetables in their routines, to focus on foods that are rich in antioxidants, and to limit fat and boost fiber.
More recently, nutritional steps have been tested not only for cancer prevention, but for cancer survival. Studies of individuals diagnosed with breast or prostate cancer have shown that diet may make a major difference in the ensuing years.
Safe and Effective Approach
Dietary approaches are often remarkably effective. The cholesterol lowering power of the diets by Drs. Ornish, Esselstyn, and Jenkins rivals that of typical cholesterol-lowering medications. Their effect on blood glucose control rivals that of oral diabetes drugs. For migraines or arthritis, not everyone improves with dietary adjustments that eliminate common dietary triggers, but many do; in controlled clinical trials, sometimes simple diet changes bring dramatic improvements.
Unlike the undesirable side-effects we associate with medications, healthful diet changes desirable side-effects. people who adjust the menu in hopes of reducing their cholesterol get the bonus of losing unwanted weight. Their blood pressure drifts downward as well. If they have diabetes, it comes under better control, and they may be able to reduce their need for medication.
While many still think of medications as "conventional medicine" and dietary changes as "alternative therapies," a growing number of clinicians would turn the definitions around. For many conditions, attention to diet and lifestyle is the foundation of good clinical care. Medications, surgery, or other treatments should be used when diet and lifestyle changes do not apply or are not, by themselves, sufficient for the task at hand.
New clinicians come to find that problems they had once regarded as strictly medical, or perhaps even genetic - diabetes and coronary disease, for example - have major nutritional antecedents. As time goes on, they start to see nutritional problems everywhere. The role of nutrition is indeed greater than most clinicians and patients realize. At the same time, not all problems have nutritional connections, and even for nutrition-related conditions, medical diagnosis and treatment have as important a role now as ever.
Unlike the undesirable side-effects we associate with medications, healthful diet changes desirable side-effects. people who adjust the menu in hopes of reducing their cholesterol get the bonus of losing unwanted weight. Their blood pressure drifts downward as well. If they have diabetes, it comes under better control, and they may be able to reduce their need for medication.
While many still think of medications as "conventional medicine" and dietary changes as "alternative therapies," a growing number of clinicians would turn the definitions around. For many conditions, attention to diet and lifestyle is the foundation of good clinical care. Medications, surgery, or other treatments should be used when diet and lifestyle changes do not apply or are not, by themselves, sufficient for the task at hand.
New clinicians come to find that problems they had once regarded as strictly medical, or perhaps even genetic - diabetes and coronary disease, for example - have major nutritional antecedents. As time goes on, they start to see nutritional problems everywhere. The role of nutrition is indeed greater than most clinicians and patients realize. At the same time, not all problems have nutritional connections, and even for nutrition-related conditions, medical diagnosis and treatment have as important a role now as ever.
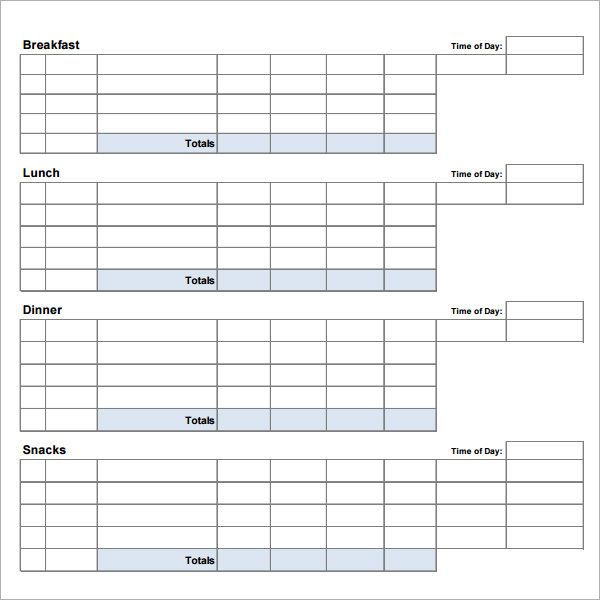
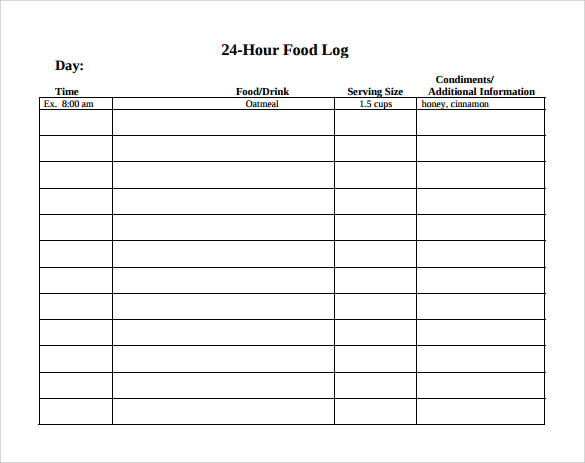
Food Consumption Timing
There could be may variations of food consumption timing that would apply to different cases and situations.
FASTING
Fasting can have therapeutic benefit with many different types:
Fasting can also vary in length:
- Two meals per day plus a snack. This means skipping lunch or dinner and/or turn it into a snack and making sure you eat breakfast.
- Time restricted eating. This is a practice of eating all food within the 12 hour window. Example is having breakfast at 7am and finishing dinner by 7pm. Another way is doing a 10 or 8 windows may be even better.
FASTING
Fasting can have therapeutic benefit with many different types:
- Water fast: drink only water - for detox and rests
- Juice fast: drink vegetable/fruit juices - for individuals needing a high antioxidant load
- Longevity fast: 800 calories, half from nuts/half from vegetables
Fasting can also vary in length:
- 24-36 hours: a good place to start
- 3-10 days: where days: where real therapeutic benefit begins
- >10 days: requires close medical supervision, usually done in a residential setting
Article Review
Video Review
|
|
|
Submit your Reflective Journal after watching the videos, reading the lesson and article.